Beagles And Epilepsy
There are some dog breeds among which epilepsy is more prevalent than in the general population. […]

Finding Out About Joints And How They Can Affect Pets
The list of joint ailments in pets, particularly dogs and cats, is almost endless. You may have noticed some or all of these symptoms and wondered what could be causing the problem. […]

Skin Diseases: What To Watch For And Issues You Can Treat!
There are several skin diseases that can affect both cats and dogs and, unless severe, can be treated at home. […]

My Cat Has Inflammatory Bowel Disease: Can I Manage It At Home?
Inflammatory bowel disease (IBD) is a chronic condition that affects the gastrointestinal tract, particularly the intestines. […]

Dealing With Your Pet’s Upset Tummy And Diarrhoea
If your cat is experiencing diarrhoea, there are several steps you can take to help them. […]

Skin Cancer In Dogs
Skin cancer in dogs is far more common than most would expect. It accounts for approximately 30% to 40% of all cancer cases reported. […]

Cancer In Dogs
For any dog owner among the grimmest of news to get is that your beloved pet has been diagnosed with cancer. […]

Caring For Your Cat’s Ears
The most common ear problems in cats are infections generally caused by bacteria, yeast, fungus, or mite infestations. If an ear infection recurs, the causes should be identified and treated to prevent more severe complications in the future. […]

Stress In Pets And Digestion
Stress in pets is real and it can seriously affect how they are nourished. Chronic stress could lead to many negative outcomes with malnutrition and digestive disorders high on the list. […]

Caring For Your Dog’s Ears
Dogs’ ears are highly vulnerable to infections and pests. The good old-fashioned advice that an ounce of prevention is worth a pound of cure applies very much to this aspect of canine care. […]

Gastrointestinal Health In Dogs And Cats
Any owner who has dealt with a pet’s sudden unexplained vomiting or diarrhoea will understand that this is a stressful experience for everyone involved. […]

Your Cat’s Digestive System
Cats are known to be finicky eaters but understanding the basics of cat digestion can help you provide your pet with the nutrients they need. […]

Canine Eye Health
Dogs’ eyes, similar to those of most animals, have the same function and design as humans’ eyes. Both are thus subject to many of the same age-related changes and ailments. […]

Caring For Your Dog’s Skin
Most dog owners know that keeping your pet in great condition starts with proper nutrition. But after that, sensible skin care can also make the difference between your dog being happy or miserable. […]

Discover The Causes Of Pain In Cats
Experts define pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage.” […]

What Causes Pain In Dogs?
Dogs will rarely cry or whine unless they are in severe pain. […]

Chronic Kidney Disease In Cats – About The Disease
CKD affects approximately 35% of geriatric cats and up to 10% of cats that visit veterinary clinics. The disease is progressive over time and occurs where there is long-standing, irreversible damage to the kidneys that weakens their ability to remove waste products from the blood and regulate other essential functions. […]

CKD A Common Disease In Domestic Cats
Chronic kidney disease (CKD) is a common, progressive and debilitating disease in cats, affecting a large number of cats crossing consulting room tables in veterinary clinics. The prevalence of feline CKD increases with age. Geriatric cats in general often develop some degree of kidney disease. […]

Causes Of Feline Chronic Kidney Disease
The feline kidneys are paired organs that reside in the dorsal abdomen. One is situated on the left and the other on the right. […]

CKD – The Silent Disease
The crucial functions of the kidneys include removing toxins and excess water from the body; maintaining water, salt and acid balance; producing hormones and maintaining normal blood pressure. […]

Pet Diabetes
What is pet diabetes? How common is diabetes in pets? What signs should I look out for? How is diabetes diagnosed? How is diabetes managed in pets? […]

What You Need To Know About Zoonotic Diseases
A zoonotic disease (or zoonosis) is a type of disease that passes from an animal or insect to a human. […]

Companion Animals and Coronavirus
There are various types of coronaviruses. This article looks at the differences between the two types you should know about. […]

Osteoarthritis In Dogs
Dogs, just like humans, can also suffer from osteoarthritis (OA), sometimes called degenerative joint disease. […]

What You Should Know About Osteoarthritis
Osteoarthritis (OA) or degenerative joint disease (DJD) is the terminology used when referring to a form of chronic joint inflammation that is a progressive and permanent disease of joints. […]

What Is Osteoarthritis?
Osteoarthritis (OA) or degenerative joint disease (DJD) is the terminology used when referring to a form of chronic joint inflammation that is a progressive and permanent disease of joints. […]

Diabetes In Cats: Symptoms
More and more cats are developing diabetes mellitus. Cat owners need to act on this alarming fact by learning more about this chronic disease. […]

The Management And Prevention Of Diabetes In Dogs
While diabetes in dogs may not be curable, it can be managed quite successfully. Here is an overview of how to manage and treat diabetes in dogs. […]

The Importance Of Catching And Diagnosing Diabetes In Dogs Early
Unfortunately, there is no cure for diabetes. That’s why it’s important to notice and address the signs of diabetes in dogs early. With treatment and proper management, a healthier and longer life is possible. […]

Diabetes In Dogs: Symptoms
The occurrence of diabetes in canines is increasing. Find out what it is and what symptoms to watch for. […]

An Overview Of Cancer Causes And Signs In Dogs
Better health care and improved nutrition have increased the average lifespan of canines. Unfortunately, with old age comes greater cancer risks. […]

Facts About Your Cat’s Heart
The body needs oxygen-rich blood. The heart makes sure this blood gets around. Then, once the oxygen-depleted blood goes through the lung fields, the cycle repeats. A cat’s heart is a small yet impressive organ which works around the clock. […]

Types Of Rare Cancers In Cats
The following tumours and cancers are rare in cats: Brain tumours, Liver tumours, Lung tumours, Mammary tumours and Nasal tumours. Read more about it here. […]

Diagnosing, Treating & Preventing Cancer In Cats
It’s important to find and treat cancer in cats as early as possible because many types of tumours in cats tend to form, grow and spread quickly. With the appropriate treatment, long-term prognosis can be improved. […]

An Overview Of Cancer In Cats
It’s unclear what causes most cancers in cats. Fortunately for cat owners, feline cancer is not as common as cancer in dogs. Still, it’s good to be aware of the signs of cancer in cats […]

10 Common Canine Cancers: Part 2
This is Part 2 of Common Canine Cancers: Read Part 1 first. […]

10 Common Canine Cancers: Part 1
Cancer is a complex disease that is unfortunately very common in both humans and dogs. It can be triggered by various things such as environmental, genetic and lifestyle factors. […]

Ear Infections In Cats: Signs, Causes, Diagnosis, Treatment & Prevention
Luckily, when it comes to ear infections, cats are not as vulnerable as dogs. Still, when they do get them, the effects can be painful and even cause damage if left untreated. […]

Ear Infections In Dogs: Treatment & Prevention
If your dog has an ear infection, it’s really important to approach the problem properly. The safest and smartest first step would be to contact your veterinarian. […]

Ear Infections In Dogs: Signs, Causes & Diagnosis
The first thing you should know is that ear infections in dogs are quite common. The important thing is to address signs and symptoms as soon as you notice them. […]

The Causes And Signs Of Yeast Infection In Dogs
Yeasts are microscopic fungi. Opportunistic fungi can increase and cause skin, paw and ear infections when the circumstances are right. The condition can be super uncomfortable and should be addressed as soon as possible […]

An Overview Of Stud Tail In Cats
If you haven’t heard of stud tail in cats, or want to know more, here’s a handy overview. […]

A List Of Common Skin Problems In Cats
Excessive grooming, head shaking and scratching can all be signs of cat skin problems. You should always pay attention and investigate when your cat’s behavioural patterns change. […]

What’s Causing Your Dog’s Skin Problems?
Nobody likes having an itchy or irritated skin and your dog is no different. Unfortunately, skin problems are very common in canines and shouldn’t be ignored. […]

A List Of Common Eye Conditions In Canines: Part 2
Welcome to Part 2 of common eye conditions in canines. […]

A List Of Common Eye Conditions In Canines: Part 1
Dogs’ eyes are very important organs that help them form images of the world. Threats to healthy eyes include injuries, conditions and diseases. […]

A List Of Common Eye Conditions In Felines
Cats have very unique and beautiful eyes. They can detect much more light than we can, however, their colour vision is limited. Threats to healthy eyes include injuries, conditions and diseases. […]

Cat Anxiety
As in humans, stress and anxiety in cats can impair the ability to function and further aggravate existing physical conditions. Any change in a cat’s environment can cause stress and anxiety. […]

Stress In Dogs
Dogs, like humans, can experience chronic stress causing a variety of physical issues that can develop into serious health problems. Prolonged stress may also affect a dog’s emotional state making him more aggressive or potentially dangerous. […]

Ear Infections In Cats
Ear infections, causing painful itchiness and irritation, are not as common in cats as they are in dogs. Although ear infections themselves are problematic, there can be underlying causes of the inflammation of the external ear canals […]

Chronic Ear Infections In Dogs
Ear infections, causing painful itchiness and irritation, are one of the most common problems afflicting dogs. Although ear infections themselves are problematic, there are usually underlying causes […]

Pain Management For Your Dog
Like humans, dogs are happier when they are healthy and pain-free. The thing is, it’s not always obvious when a dog is experiencing discomfort. It’s up to dog owners to learn about signs and symptoms of pain […]

Constipation In Cats
Constipation is the inability to routinely and easily evacuate the bowels resulting in retention of faeces or passage of hard, dry faeces. When a cat is constipated, the colon […]

Constipation In Dogs
Constipation is the inability to routinely and easily evacuate the bowels resulting in retention of faeces or passage of hard, dry faeces. When a dog is constipated, the colon […]

Abscesses In Dogs
A common skin condition in dogs is an abscess that can form if an irritation worsens or if bacteria invades the skin. An abscess can be quite unsightly and alarming and can be found on almost any part of a dog’s body. […]

Abscesses In Cats
A common skin condition in cats is an abscess that can form if an irritation worsens or if bacteria invades the skin. An abscess can be quite unsightly and alarming and can be found on almost any part of a cat’s body. […]

Acid Or Gastroesophageal Reflux (GERD) In Cats
Cats, like humans, can suffer from acid or gastroesophageal reflux disease, GERD. Acid reflux is quite common in cats and while younger cats are at greater risk, cats of all ages may be susceptible. […]

Acid Or Gastroesophageal Reflux (GERD) In Dogs
Dogs, like humans, can suffer from acid or gastroesophageal reflux disease, GERD. Acid reflux is quite common in dogs and while puppies are at greater risk, dogs of all ages may be susceptible. […]
Acute Diarrhoea In Cats
Cats with acute diarrhoea may defecate more frequently, and may have softer, looser or more watery faeces. Blood, mucus, or even parasites may be visible in or on their stools and they may have accidents in the house. […]

Acute Diarrhoea In Dogs
Dogs with acute diarrhoea may defecate more frequently, and may have softer, looser or more watery faeces. Blood, mucus, or even parasites may be visible in or on their stools and they may have accidents in the house. […]

Diabetes In Dogs
Diabetes, or diabetes mellitus in dogs, is a chronic disease caused when the body cannot properly respond to the hormone insulin, which is produced and release by the pancreas. […]

Diabetes In Cats
Feline diabetes, or diabetes mellitus, is a disease caused when the body cannot properly respond to the hormone insulin, which is produced and released by the pancreas. As in the human body, the cells in a cat’s body need […]

A Heart-To-Heart About Pet Heart Health
If you love your pets with all your heart it’s important to know more about their hearts and what may happen to this vital organ during the course of their lives. […]

Vaccinate Against Kennel Cough
Kennel Cough is an infectious respiratory disease of dogs which usually results in a persistent, dry hacking cough. Usually found in environments where there has been recent contact with a single or group of infected dogs. […]

Aspiration (Or Inhalation) Pneumonia In Dogs
Dog owners need to be aware of the risk of aspiration (or inhalation) pneumonia. What is aspiration (or inhalation) pneumonia? Aspiration pneumonia, also called inhalation pneumonia, occurs when a dog’s lungs become inflamed […]

What You Need To Know About Heart Attacks In Dogs
The heart muscle is called the myocardium. An infarction is the obstruction of the blood supply to an organ or region of tissue. Myocardial infarction, which literally means ‘heart tissue damage or death’, […]

Heart Disease In Dogs
It’s terrible to think about it, but pets can also suffer from heart problems. Congenital heart disease (heart disease that’s been there from birth) is usually picked up in puppies and is not that common. […]

Pancreatic Cancer (Adenocarcinoma) In Dogs
The pancreas is a gland organ in the digestive and endocrine systems. It is responsible for hormonal and digestive functions. Pancreatic cancer develops as abnormal pancreatic cells multiply rapidly in the pancreas. […]
Stomach And Intestinal Cancer (Leiomyosarcoma) In Cats
Stomach and intestinal cancer is also known as leiomyosarcoma, which arises from the smooth muscles of the stomach and intestines. Leiomyosarcoma is an uncommon cancerous tumor that is an extremely serious and painful disease. […]

At Home Management For Cats With CKD
Once a cat has been diagnosed with chronic kidney disease (CKD), a few things need to happen. […]

10 Tips For Cat Owners – Caring For A Cat With CKD
Stay positive, familiarise yourself with the disease, […]

Facts About A Dog’s Heart
Studies show that people who own pets are healthier, have fewer heart attacks and live longer. Happy, healthy dogs also live longer than unhealthy, unhappy dogs. […]

World Rabies Day – Awareness & Prevention Efforts
Rabies spreads when the saliva of an infected animal – through a bite or otherwise – comes into contact with broken skin (which includes scabs) or the eyes, nose or mouth of another animal or person. World Rabies Day […]

Rabies: Diagnosis, Prevention & The Value Of Vaccination
Rabies is a dangerous, fatal viral disease that can be contracted by animals and humans. Animals are typically the transmitters and dogs alone are responsible for 99% of related deaths. […]

Congestive Heart Failure (CHF) As A Result Of Dilated Cardiomyopathy (DCM)
Did you know that canine heart disease is just as dangerous in dogs as it is in people? The heart is one of the most miraculous “machines” that works like a pump and beats thousands of times per day. […]

Congestive Heart Failure (CHF) As A Result Of Atrioventricular Valvular Insufficiency (AVVI)
Did you know that canine heart disease is just as dangerous in dogs as it is in people? The heart is one of the most miraculous “machines” that works like a pump and beats thousands of times per day […]

Health Issues & Conditions In Specific Dog Breeds
A big part of a dog’s general wellbeing is their health. Unfortunately some breeds are more likely to suffer from certain conditions than others. These breeds are: Bulldogs, Beagles & Boxers. However, they’re not the only ones. […]
Eye Inflammation (Anterior Uveitis) In Cats
Uveitis is one of the most common eye disorders in cats and can be extremely serious. Without medical attention, your cat’s eyesight is at great risk. […]

What You Need To Know About Epilepsy In Dogs
Epilepsy is a brain disorder that is more common in dogs than in cats. […]

Epilepsy & Seizures In Dogs
Pets, including dogs, can also suffer from seizures. They occur when there is ‘explosive’ electrical activity in the brain and are often described as an uncoordinated firing of the neurons. Why neurons do not function normally is not understood […]

What To Do During A Dog’s Seizure
There are often warning signs when a dog is about to have a seizure. A dog may begin to act scared, dazed, stressed or anxious without cause. Dogs may also have trouble seeing, experience muscle and limb contractions, and even lose bowel and bladder control. […]

Dog Epilepsy Can Be Managed
Epilepsy in dogs is a common condition that cannot be cured, but it can be managed so your dog can have a full and happy life. Successful management requires lifelong medical attention and knowing what to do to best manage your dog’s condition. […]

Osteoarthritis In Cats
Cats are natural survivors and masters at hiding pain, which means discomfort and illness often go unnoticed. If owners and veterinarians can’t see any issues, no diagnosis can be made which means symptoms and pain caused by diseases go untreated. […]

Upper Respiratory Infections In Cats
A cat’s respiratory system consists of the large and small airways and the lungs. As a cat breathes air in through its nose or mouth, the air travels down the trachea, which divides into the tubes known as […]

Epilepsy In Dogs
Not everyone knows that dogs can suffer from epilepsy. Find out everything you need to know about epilepsy in dogs. […]

Anaemia Due To Iron Deficiency In Dogs
Anaemia is not a specific disease and doesn’t present in isolation, but is a symptom or condition that occurs as a result of other processes going on. When a dog has anaemia there is a drop in the number of red blood cells in the bloodstream. […]

Anaemia Due To Iron Deficiency In Cats
Anaemia is not a specific disease and doesn’t present in isolation but is a symptom or condition that occurs as a result of other processes going on. When a cat has anaemia there is a drop in the number of red blood cells in […]

Rabies In Pets
Whenever you hear the word ‘rabies’ you should pay attention. Mammals – for our purposes humans, dogs and cats – can all get rabies. Rabies is a deadly virus and survival is […]

Enlarged Heart (Dilated Cardiomyopathy) In Cats
Did you know that feline heart disease is just as dangerous in cats as it is in people? What is an enlarged heart? […]

Heart Disease In Cats
We don’t want to know or think about it, but cats, just like people, can also suffer from heart disease. Any disease that affects the heart muscle is called cardiomyopathy and can lead to heart failure. […]

Facts About Your Cat’s Eyes
Cats are weird, wonderful and rumoured to be wise… especially when you look in their eyes! But, how do they actually view the world around them? […]

Kidney Toxicity (Drug Induced Nephrotoxicity) In Dogs
Like human kidneys, a dog’s kidneys balance certain substances in the blood and filter out and excrete the body’s waste as urine. Some drugs administered for the purpose of diagnosing or treating another medical disorder may have toxic effects on a dog’s kidneys. […]

Anxiety In Dogs – Fears & Phobias
Anxiety or fear is the feeling that something bad or unpleasant will happen. It is related to uneasiness, nervousness, restlessness, tension and dread. […]

Rabies: How It Spreads, The Signs & Why Vaccination Is Vital
Rabies is a zoonotic viral disease, meaning a disease that normally exists in domestic and wild animals that can infect humans. It attacks the central nervous system and once symptoms develop, it’s almost always fatal. […]


HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Beagles And Epilepsy

There are some dog breeds among which epilepsy is more prevalent than in the general population.
These include:
- Belgian Shepherds
- German Shepherds
- Golden Retrievers
- Labrador Retrievers
- Miniature Schnauzers
But the breed most likely to suffer from the affliction is the Beagle. It is estimated that 2-5 out of every 100 beagles will develop epilepsy at some point in their lives.
Lafora Disease
Why this should be so, is not clearly understood. In 2022, a study was published on the clinical symptoms of twenty-eight beagles with Lafora disease, which is a rare genetic disorder that causes epilepsy. The conclusion was that Lafora disease is relatively common in beagles, with a prevalence of 2.5% in the study population.
The most common clinical signs of Lafora disease in beagles are
- Seizures
- Myoclonus (a type of movement disorder that is characterised by sudden, involuntary muscle twitches. It can affect any muscle in the body, but most commonly the legs and muzzle).
- Ataxia (a type of movement disorder that is characterised by loss of balance and coordination).
It is caused by Lafora bodies, which are abnormal protein deposits in the brain that can damage nerve cells and disrupt normal brain functions.
Early diagnosis of Lafora disease is important for providing optimal care for affected dogs because it is a progressive disease, with a mean survival time of 2.5 years after the onset of clinical signs.
The study’s authors also recommend that beagles with epilepsy undergo genetic testing for Lafora disease, as this can help to confirm the diagnosis and rule out other causes of epilepsy.
Signs of Epilepsy
If you have a beagle, it is important to be aware of the signs of epilepsy so that you can seek veterinary attention if your dog experiences a seizure.
Here are some of the signs of epilepsy in dogs:
- Loss of consciousness
- Muscle twitching or jerking
- Drooling
- Foaming at the mouth
- Chewing
- Biting
- Urinating or defecating involuntarily
- Staring
- R paddling – a rhythmic, paddling motion of the hind legs
If you see your dog experiencing any of these signs, it is important to stay calm and keep your dog safe. Clear away any objects that could injure your dog during the seizure. Do not try to hold your dog down or put anything in their mouth. Once the seizure has passed, contact your veterinarian immediately.
The most common treatment is anti-epileptic drugs (AEDs), also known as anticonvulsants. AEDs work by changing the electrical activity in the brain to prevent seizures. There are many different types of AEDs available, and your veterinarian will work with you to find the one that is most effective and has the fewest side effects for your dog.
Other treatments for epilepsy in dogs include:
Diet: Start a special diet that is high in medium-chain triglycerides (MCTs), a type of fat.
Surgery: Surgery may be an option for dogs with epilepsy that is not well-controlled with AEDs.
Vagus nerve stimulation (VNS): A device that helps control seizures is implanted.
Other actions to help manage your dog’s epilepsy
Keep a seizure diary. This will help you to track the frequency and severity of your dog’s seizures, and it can help your veterinarian to adjust your dog’s treatment plan as needed.
Identify and avoid your dog’s triggers. Some dogs with epilepsy have specific triggers that can cause them to have seizures. Common triggers include stress, excitement, and fatigue. If you can identify your dog’s triggers, you can try to avoid them to help reduce the frequency and severity of their seizures.
Be prepared for seizures. If your dog has a seizure, stay calm and try to keep them safe. Clear away any objects that could injure your dog during the seizure. Do not try to hold your dog down or put anything in their mouth. Once the seizure has passed, contact your veterinarian immediately.
With proper treatment, most dogs with epilepsy can live longer and happier lives.
Related Articles
HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Finding Out About Joints And How They Can Affect Pets

The list of joint ailments in pets, particularly dogs and cats, is almost endless.
You may have noticed some or all of these symptoms and wondered what could be causing the problem.
- Limping: In less serious cases, your pet may intermittently limp on one or both back legs, but it might get worse over time.
- Pain: Signs of pain around the hip area when they’re petted or touched there.
- Changes in Behaviour: Some pets, particularly dogs, may become aggressive or shy away when petted.
- Physical Changes: Thigh muscles could shrink, and your pet may feel pain when their hip joint is moved. One leg may also look shorter.
To better manage our understanding of the causes and treatments, in this article, we take a broad overview of the most common disorders.
Primarily, the afflictions in cats’ and dogs’ joints are either inflammatory or non-inflammatory.
INFLAMMATORY DISEASES
These occur when the body’s immune system responds without invaders to defend against, and this triggers inflammation.
In cats, this causes autoimmune conditions like Musculoskeletal Autoimmune Diseases of which examples are Immune-Mediated Polyarthritis and Rheumatoid Arthritis. If your pet has one of these, you might notice them being lethargic, limping, showing signs of muscle pain, or even losing muscle mass.
In dogs, Immune-Mediated Polyarthritis specifically targets the joints, leading to inflammation and discomfort. Often unnoticed, this internal physiological battle can significantly impact an affected pet’s quality of life.
The typical treatments for these diseases are:
- Anti-Inflammatory Medications: These drugs help lessen pain and swelling.
- Chemotherapy Drugs: These medicines work by calming down the immune system to stop it from attacking the joints.
- Physical Therapy: This includes exercises that can help improve how well the joint moves.
- Surgery: In more serious cases, an operation might be needed.
NON-INFLAMMATORY DISEASES
Aseptic Necrosis of the Femoral Head or Legg-Calvé-Perthes Disease is a condition where the blood supply to the top part of the thigh bone (femur) gets cut off. This causes the bone to break down. This condition often affects both hip joints and is commonly seen in young small dogs or puppies of small breeds and also occurs in cats.
The most common surgical treatment for both dogs and cats is called a Femoral Head Ostectomy (FHO). This procedure involves removing the head and neck from the femur. FHO surgery can be very successful in restoring pain-free joint mobility.
Degenerative Joint Disease (DJD) is another name for arthritis or osteoarthritis. It’s a condition where the cushioning (cartilage) between the joints slowly breaks down. This can happen after an infection, injury, or surgery to the joints. This allows for bone-on-bone contact which causes severe pain and erodes the contact points. Depending on the severity, the following treatments often mitigate damage to the joints and reduce discomfort.
- Losing Weight: If the pet is too heavy, helping it lose weight can take some pressure off its joints.
- Regular Exercise: Light exercise on soft surfaces can help keep the joints moving smoothly.
- Warm Compresses: Putting a warm cloth on the sore joints can help ease the pain.
- Painkillers: Certain drugs can help reduce pain and swelling.
- Surgery: In some cases, an operation might be needed.
Common in cats and dogs are forms of joint damage caused by congenital joint deformities or traumatic injury. One, the displaced kneecap is known as Luxating Patella. When the kneecap dislocates, the kneecap structure “pops out” of its normal position in the trochlear groove at the end of the femur. This can cause your pet to limp or carry the affected leg abnormally.
Medial and Lateral Luxation occur when the kneecap slides inward or outward respectively.
Treatments for this condition include:
- Limiting Exercise: Keeping the pet’s activity levels in check can help avoid making the injury worse.
- Losing Weight: If the pet is too heavy, helping it lose weight can take some pressure off its joints.
- Painkillers: Certain drugs can help reduce pain and swelling.
- Joint Supplements: These can help keep the joints healthy.
- Physical Therapy: This includes exercises that can help improve how well the joint moves.
- Surgery: In more serious cases, an operation might be needed.
By keeping a close eye on your pet’s well-being and behaviour patterns you should catch most of these afflictions early enough for your veterinarian to prescribe the best approach in dealing with them.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Skin Diseases: What To Watch For And Issues You Can Treat!

There are several skin diseases that can affect both cats and dogs and, unless severe, can be treated at home.
HERE ARE SOME EXAMPLES:
- Ringworm: Ringworm is a fungal infection that can affect the skin, hair, and nails of both cats and dogs. It is highly contagious and can be transmitted between animals and humans.
- Flea Allergy Dermatitis: This is an allergic reaction to flea saliva, resulting in a condition called flea allergy dermatitis. The bites of just a few fleas can cause intense itching, redness, and skin irritation.
- Sarcoptic Mange: Sarcoptic mange, also known as scabies, is a contagious skin disease caused by mites. It is characterised by intense itching, hair loss, and skin irritation. It typically takes about 2 to 6 weeks from the time of initial exposure for symptoms to appear. These mites burrow into the skin and cause intense itching, redness, and hair loss. Topical treatments:
Depending on the severity of the mange, you could apply a topical medication or medicated shampoo. Such products contain ingredients like benzoyl peroxide or lime sulfur, which help kill the mites and soothe the skin. Use them only as directed.
Environmental management: Mites can survive in the environment and reinfest your pet. Wash your pet’s bedding, toys, and other washable items in hot water to kill any mites present. Vacuum your home thoroughly and dispose of the vacuum bag to remove mites and their eggs. Consider limiting your pet’s access to areas where they may pick up mites.
Preventative measures: Keep your pet away from other animals that may have mange to prevent the spread of mites. Promptly treat any other pets in the household that show symptoms or have been diagnosed with mange. Regularly check your pet’s skin for signs of reinfestation or secondary infections. This may include using a cone collar to prevent scratching, keeping your pet’s skin clean, and using products like aloe vera gel or hypoallergenic moisturisers to alleviate discomfort.
- Atopic Dermatitis: Atopic dermatitis is an allergic skin condition that can affect both cats and dogs. It is caused by an overreaction of the immune system to certain allergens in the environment, such as pollen, dust mites, or certain foods. It results in itching, redness, and skin inflammation. The primary goals are to relieve itching, reduce inflammation, and prevent flare-ups. Treatment options may include:
Moisturisers: Regularly applying moisturisers helps to hydrate the skin and reduce dryness.
Topical corticosteroids: These anti-inflammatory medications are often prescribed to control itching and inflammation during flare-ups.
Topical calcineurin inhibitors: These non-steroidal medications can be used as an alternative to corticosteroids for managing mild to moderate cases.
Antihistamines: Oral antihistamines can help alleviate itching and promote better sleep.
Immunomodulators: In severe cases that do not respond to other treatments, systemic immunosuppressants may be prescribed to control inflammation.
LIFESTYLE AND SKINCARE
Implementing certain lifestyle practices and skincare routines can help manage atopic dermatitis. These may include using mild, fragrance-free soaps and detergents, avoiding hot showers or baths, wearing soft and breathable fabrics, keeping nails short to minimise skin damage from scratching, and maintaining a consistent skincare routine.
ONGOING MANAGEMENT
Atopic dermatitis is a chronic condition, and flare-ups can occur periodically. Long-term management involves understanding and avoiding triggers, monitoring and addressing skin health, and regularly consulting with a healthcare professional for guidance and adjustments to the treatment plan.
PYODERMA
Pyoderma or impetigo is a bacterial skin infection that can occur in both cats and dogs. It typically develops in areas with moisture or skin folds and can cause pustules, redness, and hair loss. Causes: Pyoderma is usually caused by bacteria, with the most common culprits being Staphylococcus pseudintermedius and Staphylococcus aureus. These bacteria are commonly found on the skin and can multiply and cause infection when the skin’s natural defenses are compromised.
Types: Pyoderma can manifest in different forms, depending on the depth and severity of the infection. Common types include superficial pyoderma, which affects the top layer of the skin, and deep pyoderma, which involves deeper layers. The condition can present as pustules, papules, nodules, or areas of moist, oozing skin. Treatment typically involves a combination of oral or topical antibiotics to target the underlying bacterial infection. In severe cases, additional therapies such as antiseptic washes, medicated shampoos, and systemic anti-inflammatory medications may be prescribed.
Prevention and management: Preventing pyoderma involves maintaining good hygiene practices, regularly grooming and cleaning your pet’s skin, managing any underlying skin conditions, and addressing factors that may contribute to bacterial overgrowth. Follow the advice of your veterinarian regarding appropriate skincare, regular bathing, and any necessary dietary or lifestyle modifications.
FOOD ALLERGIES
Both cats and dogs can develop allergies to certain ingredients in their food, resulting in skin problems such as itching, redness, and skin inflammation.
It is important to note that while these skin conditions can affect both cats and dogs, the specific symptoms, treatments, and management may vary between the two species and even among breeds. If your pet has a skin disease that your early primary treatment has nor cured, please consult with a veterinarian for an accurate diagnosis and appropriate therapy.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
My Cat Has Inflammatory Bowel Disease: Can I Manage It At Home?

Inflammatory bowel disease (IBD) is a chronic condition that affects the gastrointestinal tract, particularly the intestines.
It is characterised by inflammation and irritation of the digestive system. While the exact cause of IBD is unknown, it is believed to result from an abnormal immune response in the gastrointestinal tract.
THERE ARE TWO PRIMARY FORMS OF INFLAMMATORY BOWEL DISEASE IN CATS:
Lymphocytic-plasmacytic enteritis: This form involves inflammation of the small intestine and is characterised by an increased number of lymphocytes and plasma cells in the intestinal wall.
Eosinophilic enteritis: This form involves inflammation of the stomach and/or small intestine and is characterised by an increased number of eosinophils, a type of white blood cell, in the intestinal wall.
SYMPTOMS OF INFLAMMATORY BOWEL DISEASE IN CATS MAY INCLUDE:
- Chronic or intermittent diarrhoea
- Weight loss
- Vomiting
- Poor appetite
- Abdominal pain or discomfort
- Increased flatulence
Diagnosing IBD usually involves a combination of tests, including a thorough physical examination, blood work, stool analysis, and imaging studies such as X-rays or ultrasound. In some cases, a definitive diagnosis may require obtaining a biopsy of the intestinal tissue.
Treatments for inflammatory bowel disease in cats typically involve a multi-faceted approach, which would include those requiring a veterinarian’s prescription and those which you can undertake yourself at home.
- Medications: Depending on the severity of the condition, your veterinarian may prescribe medications such as corticosteroids or immunosuppressive drugs to reduce inflammation and control the immune response.
- Symptomatic treatment: If your cat is experiencing vomiting or diarrhoea, medications to address those symptoms, such as anti-emetics or anti-diarrheal medications, may be prescribed.
- Dietary management: Switching to a highly digestible, hypoallergenic diet can help reduce inflammation and improve digestive health. Your veterinarian may recommend a prescription diet, or a home-cooked diet specifically formulated for cats with IBD.
- Monitoring and follow-up: Regular monitoring of your cat’s condition, including check-ups and occasional blood work, is important to evaluate the response to treatment and make adjustments if needed.
It’s essential to work closely with your veterinarian to develop an individualised treatment plan for your cat, as the management of inflammatory bowel disease can vary depending on the specific needs and response of your furry friend.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Dealing With Your Pet’s Upset Tummy And Diarrhoea

If your cat is experiencing diarrhoea, there are several steps you can take to help them:
- Keep an eye on your cat’s overall behaviour, appetite, and hydration levels. If they show signs of discomfort or if the diarrhoea persists for more than a day, it’s advisable to consult a veterinarian.
- Provide fresh water. Diarrhoea can lead to dehydration, so make sure your cat has access to clean, fresh water at all times. If they are not drinking enough, you can try offering them wet food or water mixed with a bit of low-sodium chicken broth to encourage hydration.
- Adjust their diet. Temporarily switch your cat’s diet to a bland, easily digestible food to give their gastrointestinal system a chance to recover. This can include boiled chicken (without skin or bones) or plain, cooked rice. Gradually reintroduce their regular diet once the diarrhoea has resolved.
- Probiotics. Consult with your veterinarian about using probiotics specifically formulated for cats. Probiotics can help restore the balance of beneficial bacteria in the gut, promoting digestive health.
- Avoid feeding inappropriate foods. Ensure that your cat does not have access to human food, as many items can be harmful to them and worsen diarrhoea. Additionally, refrain from giving them milk or dairy products, as many cats are lactose-intolerant.
- Maintain cleanliness. Clean your cat’s litter box regularly to prevent any contamination and maintain good hygiene. This is especially important when they have diarrhoea to avoid recontamination.
If your cat’s diarrhoea persists, if it shows signs of distress or discomfort, or if you notice bloody stools, it’s important to consult a veterinarian. They can evaluate your cat’s condition, determine the underlying cause of the diarrhoea, and recommend appropriate treatment.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Skin Cancer In Dogs

Skin cancer in dogs is far more common than most would expect. It accounts for approximately 30% to 40% of all cancer cases reported.
The majority of these are benign and do not invade neighboring tissue but a small number are malignant and through metastasis can spread to other parts of the body. The difficulty is that pet owners cannot easily distinguish these forms. As such, the best approach is to seek veterinary advice if you suspect that your companion canine has a cancerous growth.
CAUSES
These diseases are often initiated by excessive exposure to the sun with ultraviolet light being the major contributor. Other causes are viral infections, immunosuppression, contact with carcinogens, and susceptibility encouraged by your pet’s genetic profile. Light-skinned and lightly furred dogs that are frequently exposed to strong sunlight for long periods are more likely to develop skin cancers than those with thicker fur and more melanin , i.e., darker skin. Unfortunately, even those with these natural and effective sunblocks have areas of the body that are less protected. The vulnerable spots tend to be on the tummy, the insides of the hind legs, around the eyes, and the tips of the ears. Dogs with a pinkish colouring around the nose and ears are also at higher risk.
TYPES OF CANINE SKIN CANCER
Three commonly encountered types of skin cancer in dogs are:
Mast cell tumours
These are cancers that develop in the mast cells of your dog’s immune system and are the cause of most skin tumours in dogs. Though the underlying processes are still being investigated, research indicates that genetic factors and body chemistry including the sex hormones, progesterone and oestrogen, can affect their formation.
Malignant melanomas
These typically occur in the mouth or on the mucous membranes (more rarely on the furry body parts) and have a tendency to grow rapidly before spreading to other organs such as the liver and lungs.
Squamous cell carcinoma
An aggressive cancer, squamous cell carcinoma, fortunately, does not spread to the lymph nodes but injures or destroys tissue around the site.
INDICATIONS AND SYMPTOMS
Different symptoms that depend on the type of cancer, will become noticeable. A good practice is to monitor the skin of aging dogs more frequently for abnormal lumps and localised swelling. These are the signs to watch out for:
- Squamous cell carcinomas: Warty blemishes that feel solid and are raised above the level of the skin.
- Mast cell tumours: Inflamed sores with a rubbery appearance.
- Melanomas: Unusually coloured swellings or bumps around the muzzle, lips, pads, and nails.
- Any inexplicable signs that your dog is in ongoing pain, such as whimpering or limping.
It’s important to note that sores or lesions related to cancer are sometimes incorrectly diagnosed as common infections.
THERAPEUTICS FOR SKIN CANCER IN DOGS
The treatments available depend on where your pet’s tumours are located, the type of cancer, and how advanced it is. Chemotherapy, surgery, and radiation therapy are among the main options available. Just as with humans, each has a range of side effects that must be considered before deciding on the best approach to take.
If you think that your dog may have a form of cancer, please consult your veterinarian who will make a diagnosis and lay out your options and associated factors. There is no advantage to be had in delaying the onset of treatment so act decisively if you have any doubts about your pet’s condition. These may be the hardest times you share with your beloved companion, but be positive because dealing with such a disease in your pet’s best interest is the greatest service you can provide.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Cancer In Dogs

For any dog owner among the grimmest of news to get is that your beloved pet has been diagnosed with cancer.
These dread diseases appear in many guises and account for almost 50 % of deaths in dogs. Such stats can lead one to assume the worst in all cases but keep in mind that a positive cancer diagnosis is not an automatic and immediate death sentence. Veterinary science, particularly canine oncology, has been boosted by pet owners allowing new therapies to be tested on their pooches when all other routes seemed to lead nowhere positive. Sadly, only a lucky few are able to participate in these studies, but the results have allowed many new treatments to be developed and these are becoming more widely available to owners. This is the first in a short series on the types of cancers that most afflict dogs. We discuss what they are, how they are diagnosed, what to watch out for, and the most effective available treatments.
Dogs aged ten and over are particularly at risk of presenting with one of the more than one hundred types of cancer that affect our companion canine population. The symptoms range from suspicious lumps and bumps to visible lesions and many other typical indicators. Sometimes these are caused by conditions other than cancer, which is why owners should have the pet checked by a vet when concerns arise. Knowing what to watch out for will help you identify a possible malignancy and arrest its progress with the help of your medical specialist.
BONE CANCERS
These originate in the bone or from elsewhere if the disease has metastasized.
Osteosarcoma is the most common form and accounts for around 95% of bone cancer cases. It occurs when immature bone cells are malformed and undergo abnormal growth. Because it is such an aggressive affliction early detection is essential. Even then the treatment is drastic, often requiring amputation of the affected limb. The good news is that catching and treating it early can allow the patient to survive in good health for several years longer.
Chondrosarcoma has the second highest incidence rate among canines and is usually located in the nasal cavities or ribs.
Another but much less common form is Myeloma also known as bone marrow cancer, which affects the white blood cells.
SIGNS AND SYMPTOMS
Loss of appetite and lethargy: If this unusual behaviour continues for more than two or three days it should be taken seriously. Of course, it isn’t invariably serious, but it is an easily spotted early warning that is wisest to address without delay.
Wobbly gait or limping and lameness: Never ignore this indication that your dog is unwell. It may not be anything more severe than a muscle injury but even that would benefit from attention. At worst it could be a much more dire early warning.
Indications of severe pain: You’ll know that your pooch is feeling sore if she whines and whimpers and her usual good nature has fled. No loving owner would ignore these signs for any but the shortest time.
Discharge from the nostrils: With four hundred times more smell receptors than a human, a runny nose is always a severe annoyance for a dog. Nine times out of ten this is just an allergy or something minor, but phlegmy or bloody discharges should be urgently dealt with.
Breathing difficulties: This could be caused by an allergy or something more serious. Laboured breathing should not be ignored, especially if it continues beyond a day or two.
Growth of a mass on the dog’s body, swellings in the ribs, spine, legs, or jaw: Unless it’s the temporary result of a knock or other known injury, any of these is a serious symptom.
The prognosis for dogs with various forms of cancer depends on the spread of the disease, its severity, and also the treatment you choose. Factors such as age, weight, and where the tumour is located will also affect the likely outcome. To ensure the best opportunities for successful treatment your veterinarian will take the time to discuss the best options for your dog.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly consult your veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Caring For Your Cat’s Ears

The most common ear problems in cats are infections generally caused by bacteria, yeast, fungus, or mite infestations. If an ear infection recurs, the causes should be identified and treated to prevent more severe complications in the future.
ALLERGIES:
If your cat has allergies, they can often lead to itchiness in the ears and around the head. Other symptoms that affect the skin could also be noticed. The allergies that most commonly affect your cat are to certain foodstuffs. E.g., fish and milk are frequent triggers, along with environmental allergens like dust mites and pollen.
EAR POLYPS:
These are tissue masses (thickened tissue) found in cats’ ears. They are not tumours or cancer but are due to inflammation. They are often at the root of non-resolving ear infections and veterinarians recommend their removal.
DERMATOPHYTOSIS (RINGWORM):
Such infections are characterised by patchy hair loss, reddening of the ears, and itchiness. Other typical symptoms include crustiness and flaking ear skin.
MITES:
Even if your moggy is fastidious about grooming, a cat’s ears can easily become a site for mite infections.
Mites can be picked up outdoors or from another pet that shares their living space. You’ll notice the problem by excessive scratching, inflammation, hair loss, and what looks like coffee grounds in the ear. If you’ve spotted these signs, you should deal with them immediately. Fortunately, humans are not susceptible to ear mites, so neither you nor your human family is at risk.
TREATING EAR MITES:
While the cleaning process is fairly simple, you may find that your cat does not enjoy the attention since their ears are extremely sensitive. These simple steps are recommended to ensure that the procedure is as efficient and stress-free as possible.
- Make sure your pet is calm and relaxed. Any kind of fuss may create tension and this will make the job harder.
- Have all the necessary gear nearby to limit excessive movements and distractions.
You’ll need some cotton wool swabs and buds, an ointment that contains pyrethrin or a similar pesticide (this kills mites on contact), or even baby oil (this smothers the mites). Such unguents also aid in removing the detritus, soothe the skin, and reduce discomfort.
Having someone to help you will be a great advantage but if not, you can go ahead on your own. Gently but firmly hold the cat under one arm so that both hands are free. Swaddling in a towel will lessen the chances of being slashed by an angry claw. One hand cups the cat’s head to expose the ear and the other applies the treated swab and allows you to use your fingers to remove the nasties in a few strokes. Repeat these steps with the other ear by placing the cat under your other arm. It may be necessary to penetrate the ear canal more deeply with an earbud but this could be trickier. If the earbud proves difficult, pour a little baby oil into the ear canal. A single application is seldom adequate to kill the mites, but a small amount every day for a week or two should do the job.
To reduce the need for repeated treatments, remove as much of the pests and grunge as possible before setting your cat loose. Once they’ve processed their outrage, it’s a good time to enjoy a special treat together to restore your relationship.
Of course, there’s no shame in taking your beloved to a professional pet groomer or veterinary clinic who’d be more practiced and at ease managing such operations.
If there are obvious injuries from previous scratching these will require separate attention. If they don’t clear up by themselves or with topical treatment in a few days, it may be necessary to see your veterinarian for an antibiotic prescription and to fit a collar.
Dealing with ear ailments as soon as they are noticed is essential because leaving such problems untreated can have serious consequences.
The contents of this post are for informational purposes only and do not constitute professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Stress In Pets And Digestion

Stress in pets is real and it can seriously affect how they are nourished. Chronic stress could lead to many negative outcomes with malnutrition and digestive disorders high on the list.
Background
All caring pet owners have noticed that their pets’ behaviour can change dramatically for the worse when they’re exposed to certain influences. Sometimes these originate from obvious sources but others can be more mysterious. A common example is your cat or dog’s fear response when confronted with a potential danger. This produces an immediate instinctive reaction that will probably pass as soon as the sensed risk diminishes. Recovery takes much longer when the animal is frequently exposed to the same fear stimulus. This type of behaviour modification could lead to profound character changes. A happy, friendly pooch could become aggressive and a moggy that was outgoing and affectionate could become withdrawn or anxious.
SOURCES OF STRESS
These are the main stress vectors and how they are introduced into your pet’s life.
- Physical –pain, accidents, trauma, over-exertion.
- Biological –viruses, bacteria, parasites, mould.
- Environmental –allergens, noise, other pollutants, heat or cold.
- Psychological – fear, depression, anxiety, trauma.
- Consumable – poorly formulated and highly processed foods, eating too much or too little, thirst.
- Chemical – toxic dusts and fumes, pesticides, herbicides, exposure to heavy metals.
UNDERSTANDING STRESS
Apart from the factors mentioned before, when a pet has to learn a new behaviour, such as dealing with unfamiliar surroundings, people, or animals, different parts of the brain are activated. The problem-solving part of the pet’s brain is the cerebral cortex. Also housed here is the limbic system which regulates a dog’s or cat’s emotional state. Particularly, when a dog is highly aroused, owners will often experience difficulties, such as it not obeying when being restrained. This is often interpreted as disobedience or a dominance display and may elicit an inappropriate response from the carer, thus adding to the problem.
STRESS AND THE HORMONAL SYSTEM
Under these conditions, cortisol, known as the stress hormone, is raised above the normal level and this increases adrenaline production. The consequences can be a weakened immune system which introduces risks of gastrointestinal and skin conditions while the blood pressure goes up, potentially contributing to heart and circulatory problems.
TACKLING STRESS
To help your pet manage stress there are a few steps you should follow to identify the source and deal with the effects. Take note of the circumstances when the pet appears stressed.
- Are there specific environmental factors involved e.g., loud noises or being kept in a small space?
- What physiological aspects play a role e.g., is the pet sick or suffering from some affliction or other?
Knowing what these triggers are will help you and your pet deal with stress when it happens and better still, avoid it as much as possible.
THE EFFECTS OF STRESS ON DIGESTION
Stress impacts on the brain and also the digestive tract due to the large number of nerves connecting them.
A stressed pet’s intestines will experience increased nerve activity. Blood may be withdrawn from the gastric functions toward the muscles, heart, eyes, and ears in preparation for either fight or flight.
This is all due to the urgent messages crisscrossing the sympathetic nervous system, which trigger these and other reactions:
- Pupils are dilated for better vision.
- Saliva is reduced.
- Bronchia in the lungs are opened up for better oxygen distribution.
- Heart rate goes up.
- Functions of the digestive system are restricted.
- The bladder relaxes.
- Cats could wail while dogs may whimper.
Depending on how powerful the external stimulus is, this confusion of signals can lead to vomiting, diarrhoea, and loss of appetite.
Much of your pet’s immune system originates in the intestinal tract. This means that when gastric problems arise because of stress, both their digestion and their body’s ability to ward off viruses and diseases becomes compromised.
Last thoughts
Not all stress is harmful. Good stress can include adventurous exercise, overcoming challenges, e.g., learning new tasks and skills, etc. Remember though that physiologically the same responses arise, so it’s advisable to be aware of how much your pet can comfortably manage.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Caring For Your Dog’s Ears

Dogs’ ears are highly vulnerable to infections and pests.
The good old-fashioned advice that an ounce of prevention is worth a pound of cure applies very much to this aspect of canine care. One of the primary sources of irritation and subsequent infections is Otodectes cynotis, the ear mite.
MITES
This critter is an almost invisibly small (less than 2 mm) parasite that inhabits the ear canals and the surrounding skin. Fortunately, they choose to live on the skin surface where they find their food and, unlike several other mite species, do not penetrate the skin. Nonetheless, they make their presence known by causing the poor pup endless misery from the itching and other irritations.
If you notice your dog pawing at his ears or shaking his head frequently, it may be an ear mite infestation that needs attention. Luckily, treatment is simple, safe, and easily obtained. Your local veterinarian or pet shop will have the necessary therapeutics in stock or will know where to get them.
The prevention of ear mite infections requires regular flea and tick prophylactics or an ear cleaning routine with one of the many specially formulated cleansers available in stores or online.
EAR INFECTIONS IN DOGS (OTITIS EXTERNA)
Mites are not the only problems that can affect dogs’ ears. Because they are furry and floppy and have an L-shaped canal that holds moisture, they are perfect traps for every kind of microbe, spore, and germ that cares to find its way in. Of course, dogs have evolved to survive these attacks but often will experience great discomfort. The typical infections are fungal, bacterial, and viral but some are also caused by physical injury to the ear canal or its surrounds. Your healthy mutt is an inveterate and indefatigable investigator, forever sticking its head into bushes and hummocks of grass, which is healthy behaviour. Unhappily, sharp objects ranging from sticks to spiky leaves and twigs can cause abrasions in the ears and these could get infected.
If your dog enjoys swimming, the risk of fluid being trapped in the ear canal is high, and of course, this creates a perfect petri dish for many infection-causing pathogens. These can all result in a condition known as otitis externa, an infection that affects the outer ear canal.
SYMPTOMS
Otitis externa causes redness and swelling, with the ear being hot to the touch and it may be painful. As you’d expect, irritants that affect the ears can seriously discomfort your pet. This manifests in headshaking, pawing at the ears or side of the head, and general irritability. Additionally, there may be a nasty discharge from the ear canal.
MEDICATION
Thankfully, there are several remedies readily available ranging from disinfectants to anti-microbial and anti-fungal medications. But the best care starts with an inspection to determine the most likely cause. If the symptoms are extreme it’s only sensible to pay your veterinarian a visit immediately. But milder ones can be treated at home. If they haven’t cleared up within a day or three don’t delay the trip any longer. Ear infections may require antibiotics to rid your pet of the underlying causes.
PROGNOSIS
With as many as one in five dogs contracting some form of ear disease, these afflictions are not uncommon. Dealing with them is a routine medical procedure and, like taking care of dental health, doing so promptly and regularly helps avoid worse complications later.
Prevention is key
It’s a good idea to learn how to clean your dog’s ears safely. This involves knowing what to do and being confident about it. You will require a fluid e.g., a saline solution or a similar over-the-counter product. Ensuring that your pup can’t shake her way out of your grip, gently fill the ear canal with the solution and then massage the base of the ear. If there is internal buildup, it should start loosening and you may hear or feel the change in consistency. Using a piece of cotton wool, probe the ear to absorb the fluids and pick out the solids and then wipe the ear with a dog-friendly disinfectant. It’s advisable not to use a cotton bud or other rigid object because it could cause an injury if the dog reacts with a vigorous headshake.
Doing this consistently will prevent unhappy outcomes, as well as strengthen the bond between you and your beloved pet.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.
Related Articles








TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Gastrointestinal Health In Dogs And Cats

Any owner who has dealt with a pet’s sudden unexplained vomiting or diarrhoea will understand that this is a stressful experience for everyone involved.
The two main causes of such symptoms, poisoning and gastrointestinal (GI) illness are frightening and upsetting. In this article, we’ll discuss GI in more detail because it is the more common.
Our pets’ body plans, especially their digestive tracts, are highly similar to ours. Without going into detail on the purpose and function of the various organs, it’s sufficient to note that all must operate in perfect unison to ensure peak health.
COMMON TYPES OF GI DISEASES
Gastrointestinal diseases that can affect the stomach, intestines, and other organs are fairly common in pets, but they can be difficult to detect early. Usually, they are only noticed once they’ve caused a variety of symptoms from loss of appetite to diarrhoea and vomiting.
The GI diseases most common among pets are pancreatitis, gastric dilatation-volvulus (GDV), and inflammatory bowel disease.
Inflammatory bowel disease: This is an inflammation of the digestive tract that can induce dramatic weight loss following uncontrollable vomiting and diarrhoea.
Pancreatitis: When the pancreas becomes inflamed this condition can cause abdominal pain, diarrhoea, and vomiting.
GDV: This causes severe pain and occurs when the stomach becomes twisted. The condition often requires urgent surgery.
REPORTING TO YOUR VETERINARIAN
As a caring pet parent, you’ll quickly notice changes in your pet’s appetite or normal gastrointestinal signs e.g., abdominal swelling or pain. In such cases, without being over-anxious, it’s wise to contact your veterinarian for an early diagnosis and initial treatment. In the event that an illness is found, this should mitigate damage to your pet’s digestive system and hasten recovery.
Once at the veterinarian, you’ll be asked about your pet’s symptoms. It’s important that you provide the required details as accurately as possible. In such situations, the owner’s description of the patient’s clinical signs can sometimes be misleading. To help the process along either the veterinarian or her technical assistant will follow a structured Q & A approach to reach the correct diagnosis.
DIAGNOSIS
The first step is usually obtaining comprehensive and accurate history to identify where in the digestive tract the disease is located since this is critical in developing the diagnostic plan.
Other questions will be more specific and relate to the signalment the owner has observed. One may be asked whether food has been jettisoned from the mouth before swallowing. This is known as dysphagia and is typical of mouth or gullet diseases. Or you may have noticed that the food has been swallowed but is regurgitated soon after without being digested.
Here are some of the other indicators you will be asked about:
- When the food is expelled, is it sudden?
- Are there usually heaving motions before regurgitation and gagging sounds afterwards?
- When did these episodes start, how many have there been, and when do they happen?
- Has the diet changed and if so, how?
- Has another veterinarian prescribed treatment and medications for this problem before and how did the pet respond to the medicine?
- Has there been weight loss while still eating well or weight loss associated with a poor appetite?
If the symptoms or their descriptions are not entirely clear, you may be asked to provide a video of what happens when your pet has an episode. This can be a tremendous aid in getting your cat or dog the urgent help it needs.
MAKING SURE THAT YOUR PET’S DIET IS OPTIMAL
In most cases, early diagnosis and treatment lead to happy outcomes. To promote your pet’s GI health your veterinarian could recommend a particular nutritional approach. This will always depend on factors like your dog or cat’s age, breed, size, activity profile, and whether its neutered or intact. Whatever you decide to do, ensure that you choose the eating plan that best suits your pet’s specific needs.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Your Cat’s Digestive System

Cats are known to be finicky eaters but understanding the basics of cat digestion can help you provide your pet with the nutrients they need.
All felines are obligate carnivores, meaning they must consume animal-based proteins to meet their nutritional needs. To select the types of food that are best for your pet, it’s important to understand how a cat’s digestion works.
The stomach of a cat is designed to digest proteins, fats, and other nutrients found in animal-based sources. The digestive system is not designed to digest grains, fruits, or vegetables. Cats also have a short digestive tract, which means that the food passes through the system quickly. This means that cats require frequent, small meals throughout the day.
A cat’s diet should consist of protein-rich foods such as meat, fish, eggs, and some dairy products. Cats also need essential fatty acids to remain healthy, so it’s important to include fatty fish such as salmon or sardines regularly in their diet. Avoid feeding your cat processed foods and human treats as these can be high in sugar, sodium, artificial flavourings, and are low in nutrition.
To ensure your cat is getting all the nutrients they need, talk to your veterinarian about the best diet for your pet. Your veterinarian can help you determine the right balance of proteins, fats, and carbohydrates for your cat’s dietary needs. Age, size, activity levels, and even the breed should be taken into account when making these decisions.
HOW DIGESTION HAPPENS
The digestive process begins in the mouth where a small amount of the amylase enzyme is present in the saliva. Once chewed, the food is swallowed and enters the gullet (oesophagus), which connects the mouth to the stomach. While no digestion takes place here, the consequences can be serious if the swallowing function is abnormal.
The stomach, which has a relatively large volume receives the chewed food and secretes gastric juices for moistening and diluting the food, acids for breaking it down, and some enzymes. On its journey, the pre-digested food leaves the stomach through the pylorus valve.
The small intestine is a long narrow passage and this is the area where the bulk of the digestion and nutrient absorption occurs. Several types of enzymes are produced by the pancreas to digest proteins, fats, and carbohydrates, which are transformed into micro units (such as amino acids) to allow absorption through the intestinal wall. The critical organs for processing fatty foods are the liver and gall bladder, which produce emulsifiers that allow fats to be carried by the blood to the cells. They also contribute to the excretion of waste products into the large intestine. This is the area where the fluid content from the liquified product of the small intestine is absorbed, thus creating a more solid substance that finally becomes the feces deposited in the kitty litter.
SIGNS OF DISORDERS
If any area in the digestive tract stops functioning normally, signs of illness will appear and these are sometimes clearly characterised by the part affected.
The Mouth: Oral diseases often cause inappetence, discomfort while chewing, hypersalivation, or a lopsided head posture when eating.
The Gullet: When this area is affected by diseases the symptoms may be loss of appetite, drooling, regurgitation, and generalised malaise. Fever may present if the lining of the oesophagus is injured and becomes infected.
Duodenum: When the small intestine stops functioning as it should, the signs generally involve the symptoms of improperly digested food, including abdominal pain, flatulence, diarrhea, bloody feces, inappetence, weight loss, and eventually malnutrition.
Colon: Problems in the large intestine match the symptoms above but are also accompanied by constipation, strained pooping, or incontinence.
Bottom: Any licking around the anus and rubbing the bottom on the ground or other surfaces, may all be present and indicate that these areas could be afflicted.
These signs may appear singly or in clusters and could also disappear before long. However, if they persist, a visit to your pet’s medical professional is advisable.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Canine Eye Health

Dogs’ eyes, similar to those of most animals, have the same function and design as humans’ eyes.
Both are thus subject to many of the same age-related changes and ailments. This means that your beloved pooch could one day suffer from a variety of ocular diseases, making it crucial to attend closely to any changes in their vision and the condition of their eyes.
Some eye conditions are genetic but many develop because of other health challenges. Diabetes, high blood pressure, and certain cancers, which have all become more common among older pets, can trigger eye disease.
Dogs often exhibit numerous indicators that they are troubled by eye problems. These could be physical, behavioural, or both together. It is known that many problems start with the ‘red eye’ symptom. You may notice colour changes on or inside the eye. Squinting, tears, and rubbing at the eyes, face, or around the head may also increase. Haziness in the eye, lots of blinking, and a nasty discharge, especially if it is gooey, could signal a disease.
Several eye diseases are commonly found among dogs and many of them can cause discomfort, sight impairment, or loss of vision. The most frequently occurring diseases endured by our canine chums are dry eye, cataracts, and glaucoma. Some eye conditions may have a genetic origin while the onset of others is linked to age or being exposed to damaging environmental factors and affect most dogs sometime in life.
Common dog eye diseases include cataracts, dry eye, and glaucoma.
Glaucoma damages the optic nerve due to increased pressure in the eyeball. This is a severe condition that can cause blindness. In humans, glaucoma mostly progresses slowly, but domestic canines get congestive or closed-angle glaucoma that develops in older days. When eye disease is identified early, treatment can manage the pain and save many dogs’ eyesight. The symptoms include swelling, redness, and pain. It should be diagnosed as early as possible and treated to avoid permanent loss of sight. Canine glaucoma can be treated surgically or with medication prescribed by your veterinarian.
Cataracts can be caused by age, injury, or certain diseases. With age, many dogs develop a haziness in the eye and this is termed nuclear sclerosis. This is a less serious condition and is seldom treated. Cataracts also appear as cloudy areas on the lens of the eye but these create physical barriers that prevent sufficient light from reaching the optic nerve and this can cause vision loss. The light that does enter is distorted and often gives a halo effect to objects. Other symptoms of cataracts include sensitivity to light, and difficulty seeing in dim light. Nowadays the condition is frequently treated by phacoemulsification which involves using ultra-high vibrations (40,000 cycles a second) to break down the offending structure. The remnants are then removed through a tiny incision. This treatment could include implanting a replacement lens that should restore virtually normal vision. For dogs, this highly successful procedure is the same as for humans.
The condition known as dry eye is caused when not enough moisture is produced to lubricate the eyeball. This particularly affects the cornea, which is exposed to the air’s drying effects. Symptoms of dry eye are squinting and pinching the lids shut. Usually, there is viscous discharge because insufficient moisture is exuded from the tear duct. Fortunately, the treatment is simple and effective depending on how cooperative your dog is. Basically, tear production is stimulated by using topical eye drops. In severe cases, antibiotics may be required to treat secondary infections.
Often owners have difficulty detecting if their pets have poor vision because dogs cope very well with any remaining sight. Timeous professional examination by a veterinarian is critical for diagnosing and treating eye ailments successfully to retain as much of your dog’s vision as possible.
Please contact your veterinarian at once if you’ve noticed significant changes in your pet’s ability to see. The earlier the diagnosis is made and treatment is begun, the more likely it is that you’ll be able to prevent potential long-term damage to your four-footed best friend’s eyes.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Caring For Your Dog’s Skin

Most dog owners know that keeping your pet in great condition starts with proper nutrition. But after that, sensible skin care can also make the difference between your dog being happy or miserable.
Here we describe some of the most common skin afflictions and the preventatives and treatments available to deal with them.
Fleas: Anyone who has seen their poor pooch desperately scratching to relieve the itching caused by flea bites knows what torment is. It’s even more frustrating when a dog loves lounging in special hidey holes outside the house. These are often ground zero for flea infestations and unless you deal with them there, the misery will eventually resume. In the meantime though, many excellent oral and dermally applied treatments can be employed to relieve the symptoms by killing the fleas already on your dog’s body.
Doggy Dandruff: This is an unsightly but painless condition. Don’t let that be a reason to avoid treating it because it is a symptom of potentially more serious underlying problems. Typical causes are allergies and dietary deficiencies that cause dry skin or an excess of natural skin oils. Before taking more drastic steps like seeking professional help, add omega-3 fatty acids easily obtained in fish oils to your pooch’s diet. Back this up with some extra brushing and in many cases, this will be sufficient treatment to get the problem under control.
Mange: Despite your efforts to provide the best care, your dog may pick up one of the two types of mange-causing mite species. The first and most likely is an outbreak of demodectic mites. These occur naturally in a pup’s hair follicles and are passed on from the mother at birth. However, certain conditions such as a compromised immune system can cause them to multiply out of control.
The second kind, sarcoptic mange, is harder to treat and much more uncomfortable because the itching is intense. This kind of mange requires specialized treatment to kill off the mites and prevent them from re-establishing themselves. Special care is required to stop the transmission of mites to other pets.
Lupus: An autoimmune disease, lupus occurs when the body’s own defence system begins to attack it. This leads to the destruction of a subcutaneous cell layer. The symptoms include scabbing and ulceration, particularly around the nose, mouth, and eyes. The treatment of veterinary patients with this disease requires the aggressive suppression of the immune system and can only be undertaken by a qualified doggy doctor.
Ringworm: This affliction is very common among humans and their pets. It is caused by three types of fungus known as dermatophytes (from the ancient Greek for skin and plant). The resulting condition is known as ringworm because the circular pattern of the raised skin resembles a nasty critter curled up beneath the skin. Fortunately, this is not the case and the unsightly affliction is often treated at home using anti-fungal remedies like apple cider vinegar, lemongrass oil, and others. If this fails, your veterinarian will recommend a suitable medication. Keeping your dog clean and dry will help contain the fungus from spreading to other parts of the body and other pets. Provide clean bedding regularly and don’t let them share food and water dishes with their four-footed housemates.
Use rubber gloves when handling a dog with a skin disorder. This will help prevent contact with the exposed skin or pathogens that can be spread to other animals, including humans. Use a disinfectant when you wash your hands after treating your pet.
Make an effort to groom your dog regularly, using a soft-haired brush and clean fingers.
Last but not least, to build up a resilient immune system make sure that your dog’s diet is complete and balanced.
The advice in this post is provided for informational purposes only and is not professional medical advice. To have your pet’s condition accurately diagnosed kindly see your veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Discover The Causes Of Pain In Cats

What is Pain?
Experts define pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage.” Pain has been seen as simply the transmission through nerves of information about damage or potential damage to parts of the body.
Pain is a defense mechanism, telling the cat that it is injured and urging it to move away from what may be causing it. Pain is very subjective and difficult to measure. In cats it is particularly difficult to detect because they hide the fact that they are in pain.
SIGNALS THAT YOUR CAT COULD BE IN PAIN
The following are some of the signs that may indicate your cat is in pain:
- Unexpected reactions when touched or approached, such as biting or scratching
- Withdrawal from family activities
- Lack of appetite
- Lethargy
- Restlessness
- Unusual vocalisation, such as moaning
- Rapid or shallow breathing
- Mobility changes, such as stiffness, inability to climb stairs, limping
- Decreased grooming and mat formation or increased grooming in specific areas
- Changes in personality
CONDITIONS AND DISEASES THAT CAN CAUSE PAIN IN CATS
The following may cause pain in cats:
- Cancer
- Arthritis
- Eye conditions
- Urinary tract blockage
- Bladder inflammation (cystitis)
- Kidney stones or bladder stones
- Inflammation of the pancreas (pancreatitis)
- Inflammation of the stomach lining (gastritis)
- Inflammation of the small intestine (enteritis)
- Oral, gum and tooth diseases or tooth fracture
- Tissue complications: tissue death or loss of blood supply
OTHER CAUSES OF PAIN IN CATS
Surgery
It’s becoming increasingly common for veterinarians to treat anticipated pain before cat surgery.
Injury
- Hit by a car
- Exposure to extreme heat or cold
- Scratched or bitten by another cat
- Eye trauma – from an accident or an attack
- Animal attack – bitten or injured by a dog or wild animal
- Feline Aortic Thromboembolism (FATE) – a complication from heart disease
- Poisoning – from human medications and food, plants, insecticides and other chemicals
- Gastrointestinal obstruction – blockage in the stomach or intestines, including from linear foreign bodies such as string, carpet or plastic
Infection
- Ear infections
- Bacterial infections
- Urinary tract infections
- Cat fight wound infections
Injuries and infections tend to be more common in outdoor cats.
DIAGNOSIS OF PAIN IN CATS
Your veterinarian will give your cat a physical examination to determine any obvious causes, such as an injury. Based on the examination and history, diagnostic tests will be performed.
Tests may include the following:
- Complete blood count (CBC)
- Biochemical profile to check for infection and systemic illnesses
- X-rays
- CT scans
- MRIs of any area that is identified to be feeling pain
- Ultrasounds of both the heart and the abdomen
- Biopsy of the tissue
TREATMENT OF PAIN IN CATS
Once your cat’s pain has been narrowed down, your veterinarian can begin proper treatment to resolve your cat’s discomfort.
PAIN MEDICATIONS
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can play a vital role in pain relief for cats.
- Opioids are used for more severe pain.
- Corticosteroids are used to reduce arthritic or allergic discomfort.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What Causes Pain In Dogs?

Pain in Dogs
ANIMALS OFTEN MASK PAIN
Dogs will rarely cry or whine unless they are in severe pain. They often suffer in silence because from a survival point of view, they do not want to draw the attention of predators.
It’s often difficult to identify pain but untreated pain can have system-wide damaging effects.
CAUSES OF PAIN
We can assume that a dog will experience pain following injuries or surgical procedures; however, there are many other causes of pain. Although the signs are subtle, careful observation of behavioral and physical changes will often reveal that the dog is in pain. Here’s an overview of various causes of pain in dogs:
Age
Age is often accompanied by chronic, painful and progressively deteriorating conditions that include:
- Osteoarthritis (or degenerative joint disease) – a common form of arthritis in dogs. This painful joint disease is a progressive inflammation of the joint caused by the deterioration of cartilage. This commonly occurs in middle-aged to older dogs.
- Obesity – excess weight puts more strain on bones and joints and brings an increased risk of diabetes, heart disease, high blood pressure and cancer.
- Congestive heart failure(CHF) refers to the heart’s inability to pump adequate blood to the body. There are many causes of CHF in dogs. The two most common causes are:
- mitral valve insufficiency (MVI) – a leaky mitral valve
- dilated cardiomyopathy (DCM) – a disease of the cardiac muscle that results in a decreased ability of the heart to pump blood through the body.
- Kidney issues – chronic kidney disease (CKD) is the result of the ‘wearing out’ of the kidney tissues and is an irreversible and progressive deterioration of renal function. The kidneys’ crucial functions of removing waste products from the blood stream, regulating the levels of certain essential minerals such as, potassium and sodium, conserving water, and producing urine are compromised.
Conditions
There are many conditions and diseases that cause pain in dogs. Here are just a few:
- Arthritis – the smooth cartilage covering a dog’s joints can break down and painful wear and tear lead to arthritis.
- Pancreatitis – the pancreas helps digest food and controls blood sugar. When the pancreas becomes inflamed there can be sharp pain.
- Cancer – dogs are at risk of developing various types of cancer; however, bone cancer, is one of the most painful.
- Periodontal disease or gum disease – is a progressively degenerative condition that is an inflammation or infection that causes weakening of support structures of the teeth leading to loosening or loss of teeth.
- Intervertebral disc disease – this is a painful condition as a result of an acute rupture of an intervertebral disc of the spine in the back or neck. This condition can lead to permanent spinal cord damage causing partial or complete paralysis.
Infections
Common bacterial infections in dogs include:
- Ear infections – in puppies ear mites can also be a source of infection
- Skin infection – external signs are usually present
- Leptospirosis – from drinking stagnant, contaminated water
- Kennel cough – a familiar, highly contagious disease that affects the respiratory system
Yeast infection, the most common type of ear infection in dogs, can also be painful.
Injuries
- Hit by a car
- Bitten by another dog
- Eye trauma – corneal scratches or ulcers, perforations and globe rupture
- Ingesting foreign objects – e.g. broken glass, rocks, sand or shoes
- Poisoning – from human medications, household chemicals, common foods and plants
- Back problems – back pain is a common condition in dogs as a result of activities such as, excessive leaping on and off furniture, jumping, running and other motions
- Cruciate ligament ruptures – torn knee ligament
- Broken or torn nails – usually from nail neglect
If you suspect your dog is in pain, contact your veterinarian immediately. Early diagnosis and prompt pain management protocol can provide consistent pain relief and in the case of disease slow down its progression for a good quality of life.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Chronic Kidney Disease In Cats – About The Disease

Definition of Chronic Kidney Disease (CKD)
CHRONIC KIDNEY DISEASE (CKD) IS DEFINED AS THE PRESENCE OF FUNCTIONAL AND/OR STRUCTURAL ABNORMALITIES OF THE KIDNEYS THAT PERSIST FOR MORE THAN 3 MONTHS*.
The disease is progressive over time and occurs where there is long-standing, irreversible damage to the kidneys that weakens their ability to remove waste products from the blood and regulate other essential functions.
CKD affects approximately 35% of geriatric cats and up to 10% of cats that visit veterinary clinics.
*It’s rare to discover structural or functional causes of kidney disease in early stages in cats because the initial diagnosis is normally only made in advanced stages of the disease.
HIGHLY COMPLEX KIDNEYS ARE ESSENTIAL FOR BODILY FUNCTIONS
The kidney is a remarkable organ that provides the following vital functions:
- Filtering waste products and extra water from the blood so that they can be excreted in the urine. This process eliminates toxins from the body and maintains a proper level of hydration.
- Regulating electrolytes (such as sodium, potassium, phosphorous, and calcium) in the body.
- Producing and concentrating urine, which is made up of waste, toxins, and extra fluid that the body doesn’t need.
- Producing erythropoietin, a hormone that stimulates the bone marrow to create new red blood cells. Red blood cells carry oxygen throughout the body.
- Producing renin, an enzyme that controls the body’s blood pressure.
MOST CKD CASES ARE IDIOPATHIC
Most cases of CKD have an unknown underlying cause (idiopathic); however, some conditions have been recognised as causes. These include:
- Kidney stones: Disease, genes or bacterial infection can cause kidney stones to form
- Kidney blockage: Pieces of kidney stones that have fractured or splintered can cause partial or complete blockage in the urine-carrying tube (ureter) that connects kidneys to the bladder
- Kidney tumors: Cancer, for example lymphoma (solid tumor of white blood cells) can affect the kidneys
- Infections: Bacterial infection of the kidneys may lead to sufficient damage to cause CKD
- Toxins: Antifreeze is a toxin that gets lots of attention, but there are many things in and around the house that are dangerous when ingested; for example, true lilies (all parts and even the water it’s in) and various medications (common over-the-counter and prescribed meds)
- Glomerular disease: This refers to inflammation of the glomeruli (individual units within the kidneys that filter the blood). When they are inflamed over a period of time, this can lead to CKD. Infections such as FIP/FeLV or cancer can cause the kidneys’ filtration mechanism (glomerulus) to become inflamed which causes damage that ultimately leads to CKD
- Protein problem: Amyloidosis, caused by chronic inflammation in other body parts, is a disease that can affect kidney function; normal tissue is replaced with protein deposits that can’t be cleared and tissue that suffered damage can’t be replaced
- Familial kidney disease: ‘Fancy’ cat breeds, seen mainly in Persian and related cats, have been found to suffer from irreversible hereditary diseases such as amyloidosis and polycystic kidney disease (fluid-filled cysts)
- Tubulointerstitial disease: This disease – that damages kidney tubules and causes inflammation – is difficult and dangerous to test for and because the cause is often unknown, custom treatment is rarely possible
Other conditions such as birth defects affecting the kidneys and trauma may also cause CKD. Age and lack of proper nutrition and bad food choices can be contributing factors.
In most cases, causes cannot be identified so treatment is aimed at management of the disease and complications that arise from it.
CLINICAL SIGNS OF CKD
Signs of CKD can take months or years to manifest. These may include:
- Loss of appetite
- Weight loss
- Drinking and urinating more than usual
- Dehydration
- Lack of grooming
- Dull and/or matted coat
- Dull eyes
- Sleeping more than normal
- Weakness and bad breath
- Intermittent vomiting and constipation may also occur
Some of these symptoms can of course be attributed to other diseases, so rather speak to your veterinarian and have your cat tested before jumping to conclusions.
DIAGNOSING CKD
Blood and urine tests can help diagnose CKD based on elevated levels of certain components in these fluids. Blood pressure is typically checked too. Clinical signs should be taken into consideration as well, including poor body condition / evidence of muscle wastage, small/asymmetrical kidneys and enlarged bladder.
TREATMENTS VARY
Your veterinarian will base the treatment of CKD on the test results whether they be blood tests or other biological indicators. A treatment protocol will be established that may include medications aimed at resolving specific abnormalities. A diet change including supplementation may also be recommended. With proper monitoring and treatment, your cat may have several years of good quality of life.
MANAGEMENT CHALLENGES
- Fluid Intake: Dehydration needs to be avoided. Talk to your vet about your plan of action.
- Food: Quality, balanced cat food can be pricey, but the long-term benefits are usually significant.
- Diet: Healthy cats typically require high amounts of protein, moderate amounts of fat and a minimal amount of carbohydrates. They also need other nutrients such as vitamins, minerals, fatty acids and amino acids. In cats with CKD, the ratios of nutrients usually need to be adapted.
- Toxins: You can’t follow a cat 24/7, especially if it enjoys exploring, so exposure to toxins is a big risk. Some household products or even natural organisms, such as lilies, can be dangerous.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
CKD A Common Disease In Domestic Cats

AN OVERVIEW OF CHRONIC KIDNEY DISEASE (CKD)
Chronic Kidney Disease (CKD) is a very common debilitating disease in cats. It is a progressive irreversible deterioration of kidney function or structure in one or both kidneys. The prevalence of feline CKD increases with age and geriatric cats in general often develop some degree of kidney disease.
The kidneys of cats with CKD are characterised by reduced numbers of functioning nephrons (the microscopic structural and functional units of the kidney that filter blood, return needed substances to blood and remove wastes).
CKD is a disease for which we have no cure, only the ability to slow it down and manage the other symptoms. Ultimately, it’s fatal. But there is also good news: with early and proper care and treatment, many cats who are diagnosed with kidney disease can do well for up to several years after diagnosis.
CKD IS A PROGRESSIVE, DEGENERATIVE DISEASE
Feline CKD is a progressive, degenerative disease that cannot be cured since the damage to the kidney that is characteristic for CKD is irreversible; however, with the right treatment, it can be managed very successfully for many years without affecting the special bond between cat and owner.
CKD is a concern because:
Firstly: It’s a leading cause of death and is very common in older cats and certain breeds.
Secondly: There are seldom signs until stage III is reached.
Thirdly: Even though kidneys are resilient, ongoing damage eventually affects quality of life.
FOUR STAGES OF CKD
The International Renal Interest Society (IRIS) developed a method to gauge the severity of the disease in four stages. Stage 1 is the least severe and Stage 4 is the most severe. Staging the disease is useful for treatment and monitoring of patients.
Stage I: Early kidney insufficiency
- This means that the cat’s kidney function is somewhere between 33 and 99%. It is difficult to identify kidney disease until later stages.
- Most cats who are diagnosed with stage I CKD can have several years before it progresses to stage II CKD, but every cat progresses at a different rate.
Stage II: Late stage kidney insufficiency
- This stage means that the cat’s kidney function is somewhere between 25 and 33%. The kidneys are still adequately filtering out toxins and waste products, but they are starting to struggle.
- Some symptoms at this stage may be more water intake, and a little more urine output and hypertension.
Stage III: Early kidney failure
- This stage means that the cat’s kidneys are now functioning between 15% and 25%. At this point, the kidneys are no longer able to adequately filter out all of the toxins and waste products of the body, and the cat may be starting to develop more noticeable symptoms of kidney disease.
- The primary symptoms are increased drinking and urination, increased nausea, which will usually manifest as decreased appetite, being pickier with foods, and an increase in vomiting.
Stage IV: End stage kidney failure
- This stage means that the cat’s kidneys are now functioning at less than 15%.
- The focus is on supportive care and increasing quality of life.
- The primary symptoms at this stage are extreme nausea, to the point of not eating, and lethargy.
CAUSES OF FELINE CKD
There are many possible underlying causes of CKD in cats, ranging from congenital abnormalities and immune-mediated disease to hypertension. Some chronic conditions that are common in cats such as high blood pressure and hyperthyroidism may cause CKD. However, for many cats with CKD, the cause is unknown.
However, by far the most common underlying cause in cats is tubulointerstitial nephritis – a kidney condition characterised by swelling in between the kidney tubules. In many situations in cats, this abnormality causes a progressive decrease in the glomerular filtration rate (GFR) over time, ultimately resulting in azotemia (i.e. abnormally high levels of nitrogen containing compounds such as urea and creatinine in the blood).
Chronic kidney disease (CKD) is the result of various kinds of damage to the kidneys and is very closely related to age. There are some known triggers for kidney failure, but often no precise cause is identified.
Triggers for CKD may include:
- Abdominal trauma that can damage the organs
- Certain medications
- Exposure to toxins, such as heavy metals (mercury, lead and thallium)
- High blood pressure
- Chronic urinary tract obstruction
- Chronic bacterial infection of the kidneys
- Immune system disorders, such as systemic lupus
- Some infectious diseases, such as feline leukemia and feline immunodeficiency virus (FIV)
- Congenital polycystic kidney disease
- Malformation of the kidneys at birth
BREED PREDISPOSITIONS
Some breeds reported to be disproportionately affected by CKD include:
- Persian
- Siamese
- Burmese
- Abyssinian
- Maine Coon
- Russian Blue
SOME COMMON CLINICAL SIGNS OF CKD
The most frequently observed clinical signs of CKD in cats may include:
- Increased thirst and dehydration – diseased kidneys have trouble concentrating urine and lose a lot of water
- Increased urination – when the kidney’s filters are damaged, it can cause an increase in urination
- Nausea – many of the waste products that build up in the blood of cats with CKD make them feel sick and lethargic
- Poor appetite – a side effect of nausea, most cats don’t want to eat when they don’t feel well
- Weight loss – cats with CKD often lose both muscle and fat as a consequence of poor appetite
- Other reported clinical signs are mainly related to the gastrointestinal tract and include intermittent vomiting, constipation and halitosis
TREATMENT GOALS
The goals of treatment of CKD are:
- Slow progression of the disease by controlling the buildup of waste products in the blood
- Delay the progression of the disease
- Maintain or improve the quality of life of the cat, and extend lifespan
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Causes of Feline Chronic Kidney Disease

OVERVIEW OF THE FELINE KIDNEY
The feline kidneys are paired organs that reside in the dorsal abdomen. One is situated on the left and the other on the right. The kidneys at birth are the same kidneys for the rest of a cat’s life. They don’t regrow, and ‘healing’ of damage is a limited ability for this important organ.
Kidneys are essential for normal bodily functions. The kidney is a highly complex and remarkable organ. During the day, the body makes waste that it cannot use and adds it to blood for transport to the kidney. The kidney then filters the waste products and extra water from the blood so that they can be excreted in the urine. This process eliminates toxins from the body and maintains a proper level of hydration.
Other functions of the kidneys include:
- Regulating electrolytes (such as sodium, potassium, phosphorous, and calcium) in the body.
- Producing and concentrating urine, which is made up of waste, toxins, and extra fluid that the body doesn’t need.
- Producing erythropoietin, a hormone that stimulates the bone marrow to create new red blood cells. Red blood cells carry oxygen throughout the body.
- Producing renin, an enzyme that controls the body’s blood pressure.
CHRONIC KIDNEY DISEASE (CKD)
‘Chronic’ means long-lasting; therefore, chronic kidney disease means that there is a progressive decline in the kidneys’ ability to function over time. It is not usually until the disease is fairly well advanced and the condition has become severe that signs and symptoms are noticeable. Unfortunately, at this point most of the damage is irreversible. Because the kidneys impact other areas of the body, the changes that occur as a result of chronic kidney disease impact many other bodily systems, as well.
CKD is a common problem in cats. CKD can be seen in cats of any age, but is most common in middle to old-aged cats.
BREED PREDISPOSITIONS
Some breeds reported to be disproportionately affected by CKD include: Maine Coon, Abyssinian, Siamese, Russian Blue, Oriental shorthair, and Burmese cats.
CAUSES OF CKD IN CATS
There are many possible underlying causes of CKD in cats, ranging from congenital abnormalities and immune-mediated disease to hypertension. Some chronic conditions that are common in cats such as, high blood pressure and hyperthyroidism may cause CKD.
Old age, undiagnosed and untreated health problems, diseases and unidentified causes can all lead to long-standing, irreversible damage to the kidneys.
Most cases of CKD have an unknown underlying cause (idiopathic); however, some causes are well recognised. These may include:
- Kidney stones: Disease, genes or bacterial infection can cause kidney stones to form
- Kidney blockage: Pieces of kidney stones that have fractured or splintered can cause partial or complete blockage in the urine-carrying tube (ureter) that connects kidneys to the bladder
- Kidney tumours: Cancer, for example lymphoma (solid tumour of white blood cells) can affect the kidneys
- Infections: Bacterial infection of the kidneys may lead to sufficient damage to cause CKD
- Toxins: Antifreeze is a toxin that gets lots of attention, but there are many things in and around the house that are dangerous when ingested, for example, true lilies (all parts and even the water it’s in) and various medications (common over-the-counter and prescribed meds)
- Glomerular disease: This refers to inflammation of the glomeruli (individual units within the kidneys that filter the blood). When they are inflamed over a period of time, this can lead to CKD. Infections such as FIP/FeLV or cancer can cause the kidneys’ filtration mechanism (glomerulus) to become inflamed which causes damage that ultimately leads to CKD
- Protein problem: Amyloidosis, caused by chronic inflammation in other body parts, is a disease that can affect kidney function; normal tissue is replaced with protein deposits that can’t be cleared and tissue that suffered damage can’t be replaced
- Tubulointerstitial disease: This disease damages kidney tubules and causes inflammation
Other conditions such as birth defects affecting the kidneys and trauma may also cause CKD. In most cases, causes cannot be identified so treatment is aimed at management of the disease and complications that arise from it.
Chronic kidney disease in cats can be successfully managed to offer a better quality of life.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
CKD – The Silent Disease

Chronic kidney disease is a progressive disease
Chronic Kidney Disease (CKD) is mostly a progressive disease and clinical signs are initially unnoticeable or subtle and mild. It is recognised that around two thirds to three quarters of the total functioning kidney tissue (of both kidneys) can be lost before signs of CKD will develop. Because the disease is progressive with a gradual decline there is often no diagnosis or treatment. As a result, the disease becomes chronic leading to a series of health problems. When the kidneys are weakened, the results can be devastating.
CRUCIAL KIDNEY FUNCTIONS
The crucial functions of the kidneys include:
- Removing toxins and excess water from the body
- Maintaining water, salt and acid balance
- Producing hormones
- Maintaining normal blood pressure
Unfortunately, CKD signs will worsen over time and others may arise due to accumulation of toxins in the blood or complications from the body trying to adapt to the disease.
FOUR STAGES OF FELINE KIDNEY FAILURE
It is recognised that kidney disease has four stages. They are:
Stage I: Early Insufficiency
Kidney function is estimated at lower than 99%, but higher than 33% and seeing clear symptoms are abnormal. In most cases, only tests can diagnose stage I kidney disease. It’s not a stage that should cause panic, but lifestyle improvements are recommended if a diagnosis has been made.
Stage II: Late Stage Insufficiency
In stage two, kidney function drops to roughly as low as 25%. They can still do their job, but it’s getting harder. In some cases, water intake and urination already increase. High creatinine levels, low electrolyte levels and high blood pressure can lead to diagnosis. Treatment should start once diagnosis is made.
AS CKD PROGRESSES, SYMPTOMS ARE NO LONGER SILENT
Stage III: Early Kidney Failure
Function can drop to as low as 15%. Tests may also show higher creatinine levels than before and abnormally low electrolyte levels. The following symptoms are likely to start showing because the kidneys can no longer properly play their role:
- Dry fur
- Eating less
- Less active
- Weight loss
- Increased drinking
- Increased urination
- High blood pressure
- Secondary bladder infections
- Increased nausea (fussy, eating less and vomiting)
Comprehensive treatment is crucial at this point.
Stage IV: End Stage
When this stage is reached, kidney function is lower than 15% and life expectancy is less than a year. With even more painful symptoms and increased severity of existing symptoms, quality of life is very poor. Unfortunately, you may have to make a decision about your cat’s future.
EARLY DIAGNOSIS AND MANAGEMENT FOR BETTER QUALITY OF LIFE
Routine screening of all mature and older cats can help early diagnosis so that treatment and management of the disease can be initiated to prolong a good quality of life.
The only way you can get ahead of kidney disease in cats is through routine veterinary monitoring and regular testing (yearly or twice yearly). Urine and body weight should be monitored at each visit.
Early signs that CKD may be present is a decline in urine concentration or body weight. Tests for CKD may include:
- Urinalysis
- Bloodwork (measuring urea, creatinine and/or SDMA)
- Ultrasounds
- X-rays
The goal is to delay, manage and treat irreversible conditions, such as chronic kidney disease as early as possible. Management and treatment can improve the quality of life of cats with CKD and also slow the progression of the disease.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Pet Diabetes

What is diabetes?
Diabetes mellitus (DM) is a chronic disease characterised by elevated blood sugar (glucose) levels. Insulin is the hormone responsible for lowering blood glucose and is produced by a digestive organ called the pancreas. In veterinary medicine DM can be divided into two different types; type 1 DM (insulin-dependent diabetes) or type 2 DM (non-insulin-dependent diabetes).
Type 1 DM – caused by the inability to produce sufficient insulin and is most commonly seen in dogs.
Type 2 DM – caused by the body becoming resistant to the effects of insulin or an insufficient production of insulin and is seen most commonly in cats.
How common is diabetes in pets?
A five year study published by the University of Queensland demonstrated a prevalence of 7.4 per 1000 cats, the incidence was significantly higher amongst the Burmese cat population. Risk factors include obesity, age (cats over seven appear at higher risk), breed, physical inactivity, gender and some medications.
In dogs one study reported a 0.34% incidence with certain breeds such as Cairn Terriers and Samoyed breeds over represented. In dogs DM can also occur secondary to other conditions such as pancreatitis, oestrus and Cushing’s disease.
What signs should I look out for?
The clinical signs of DM, regardless of type are the same: increased thirst, urination and hunger, inappropriate urination, weight loss, lethargy, weakness, poor skin and coat condition. In dogs, cataracts and blindness may also result.
How is diabetes diagnosed?
Diagnosis is confirmed by blood and urine testing.
How is diabetes managed in pets?
The management solution of both DM type 1 and 2 involves twice daily injections of insulin, consistent meals and exercise. Pets with type 1 DM will required life-long injections however there is an approximately 50% chance of remission for pets with type 2 DM provided early diagnosis and adequate management. Dogs and cats with well controlled diabetes can go on to lead normal lives and have the same life expectancy as non-diabetic dogs and cats.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What You Need To Know About Zoonotic Diseases

A zoonotic disease (or zoonosis) is a type of disease that passes from an animal or insect to a human. Zoonotic diseases are caused by a pathogen such as a virus, bacterium, fungus or parasite and transmitted through a ‘vector’ (e.g. mosquito, tick) in order to infect a human.
Some zoonoses don’t make the animal sick, but will make a human sick. The infected human typically transmits the infectious agent to at least one other human, who, in turn, infects others. It may range from a minor to short-term illness or to a major life-changing illness.
Zoonoses have different modes of transmission:
- Enteric zoonoses are generally transmitted through contaminated food or water and cause gastrointestinal illness such as Salmonellosis, Campylobacter and Giardia infections.
- Non-enteric zoonoses is a grouping of vector-borne diseases and infections transmitted between animals and humans and may be a bacterium, a virus, a fungus or other communicable disease agent, such as Lyme disease, West Nile virus (WNV) and plague.
- Direct zoonoses the disease is directly transmitted from animals to humans through bites and saliva (rabies) or through media, such as air (influenza).
- Environmentally mediated zoonoses (such as Anthrax, Echinococcosis, Leptospirosis), are important re-emerging infectious diseases that affect humans worldwide.
- Humans can suffer from several food-borne helminth zoonotic diseases, (such as Toxoplasmosis, Trichinellosis). The route of infection is normally consumption of the parasite’s natural host as a human food item (e.g. meat). Inadequate knowledge of infection and hygiene, and unsafe management and disposal of animal waste products facilitate transmission.
Some of the most serious zoonoses are spread by mosquitos and ticks.
The most common zoonotic diseases in South Africa are:
- Ringworm is a highly contagious fungal infection of the skin or scalp and spread by skin-to-skin contact or by touching an infected animal or object.
- Sarcoptic mange (also called Scabies) is a highly contagious, intensely itchy skin condition caused by a tiny, burrowing mite, which spreads quickly through close physical contact from pets to people.
- Giardia (also called beaver fever) is an intestinal infection caused by a giardia parasite and spreads through contaminated food or water or by person-to-person contact. Giardia is found on surfaces or in food, soil or water that has been contaminated with feces from infected animals or humans.
- Cat scratch disease (CSD) is caused by a bacterium called Bartonella henselae, which may be carried in the saliva of infected cats and in the bodies of cat fleas. This bacterial infection is usually transmitted from cat to human via scratches, although it can also be transmitted via bite wounds or when a cat licks the open wounds of a person.
- Roundworms & Hookworms are some of the most common intestinal parasites seen in both dogs and cats. Contact with contaminated soil or dog feces can result in human ingestion and infection.
- African Tick-Bite Fever (ATBF) is a bacterial infection that is spread through the bite of ticks infected with the Rickettsia africae bacteria. Ticks that are infected with tick-bite fever are usually most active from November through April. It is important to use a tick preventive product on your pets to prevent them from bringing ticks into your home.
- Toxoplasma (rare) can be transmitted to humans through ingestion of raw or inadequately cooked contaminated meat, exposure from infected cat feces, or mother-to-child transmission during pregnancy.
- Rabies is usually spread through the bite or saliva of a rabid animal. In South Africa most cases of human rabies follow dog bites. Wildlife animals most likely to spread rabies include the bat-eared fox (Namibia and North-Western Cape), black-backed jackal (Northern Province) and yellow mongoose (Highveld and Karoo). Domestic animals such as cattle and cats are sometimes infected by bites from these animals and people may then in turn be exposed to the virus as such. It is compulsory to vaccinate all dogs and cats against rabies in South Africa.
- Leptospirosis is considered the most widespread zoonotic disease in the world. It is a bacterial disease that can pass from animals to humans when an unhealed break in the skin comes into contact with water or soil where an infected animal’s urine is present.
- Bordetella the main bacteria Bordetella Bronchiseptica is a respiratory pathogen commonly found in companion animals and can cause infectious bronchitis in dogs and other animals. It can infect humans and is only a risk factor for people with weakened immune systems.
Related Articles
Vital Reasons Why You Should Clean Up After Your Dog Read Now
How To Protect Your Dogs And Family From Pests And Parasites Read Now
Good Hygiene Practices For Humans To Avoid Parasite Infestation Read Now
The Scary Thing About Sandboxes Read Now
How Tapeworms Affect Pets & Their Owners Read Now
Cat Parasites That Can Infect Humans Read Now

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Companion Animals and Coronavirus

There are various types of coronaviruses. This article looks at the differences between the two types you should know about.
Coronaviruses You Should Know About Now
- COVID-19– A viral respiratory illness in humans caused by a new type of coronavirus that doesn’t affect animals.
- Canine Coronavirus– A highly contagious intestinal infection in dogs which doesn’t affect humans. There is a vaccine for canine coronavirus, but it doesn’t prevent or treat COVID-19 in humans.
Can Companion Animals SPREAD Coronavirus (COVID-19)?
According to the World Health Organization (WHO), there is currently no evidence that companion animals such as dogs or cats can become infected with the new coronavirus (COVID-19).
Can Companion Animals TRANSMIT Coronavirus (COVID-19)?
Since pets are fomites, they may be able to transmit COVID-19 to humans.
A fomite is a surface that can transmit disease and almost anything can be a fomite. Examples of fomites include: phones, door handles, bags, cars, clothing… and pets.
So, if a person who has COVID-19 sneezes or coughs on their hand and then touches their pet, the disease can be transmitted to the pet.
How to Prevent Transmission Via Fomites
Wash your hands with soap and water as often as necessary, including before and after petting, feeding, handling, or having any other contact with animals, their living spaces, or their waste.
What to Do if You and Your Pet are Both ill During this Time of Crisis
If you are ill and your pet needs veterinary care, please call the veterinarian or emergency clinic you wish to visit first to discuss next steps.
What Can Pet Owners Do to Protect Their Pets at This Stage?
- Firstly, like everyone else, you as a pet owner should try to stay as healthy and safe as possible. That means taking the necessary hygiene steps and avoiding risks.
- Secondly, when planning for the future, whatever your current health status, make sure you include your pets in your plans.
Related Articles
What Are Pet Vaccines And Why Are They Important Read Now
World Rabies Day -Awareness & Prevention Efforts Read Now
Rabies: Diagnosis, Prevention & The Value Of Vaccination Read Now
Be a Good Puppy Owner, Don’t Miss Vaccinations Read Now
Rabies: How It Spreads, The Signs & Why Vaccination Is Vital Read Now

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
OSTEOARTHRITIS IN DOGS

Arthritis and Osteoarthritis in Dogs
Dogs, just like humans, can also suffer from osteoarthritis (OA), sometimes called degenerative joint disease.
- Arthritis is the medical term for inflammation (swelling) of the joints.
- Osteoarthritis refers to chronic joint inflammation caused by deterioration of joint cartilage surrounding the joints. Osteoarthritis is usually progressive and permanent. Older dogs are at the highest risk.
How Does Osteoarthritis Affect Dogs?
When dogs suffer from osteoarthritis, their joints become inflamed, swollen and painful. The hips, knees, elbows, shoulders and spine are the bones and joints which are most commonly affected. Dogs with mild OA may have (and show) slight stiffness of the joints. When the disease is more severe, there is often limping and an abnormal stance (called lameness).
Consequences of Untreated Pain
If pain is left untreated, most dogs with OA experience loss of mobility (limitation of movement). Untreated pain may have many damaging system-wide consequences, such as immune suppression, digestive troubles, insomnia and anxiety. It is important for pet owners to learn to recognize possible signs of pain in their pets and consult a veterinarian.
There is effective treatment available that brings pain relief.
What Causes Osteoarthritis?
Some dogs are more likely than others to develop OA.
Common causes include:
- Old age
- Obesity
- Genetic reasons
- Trauma or injury
- Excessive physical activity
- Larger breeds are more susceptible to different forms of skeletal disease than smaller dogs
- Inherited developmental abnormalities of the bones and joints
What are Signs of Osteoarthritic Pain?
Since dogs cannot easily tell us that they are in pain and signs may be subtle, it’s difficult to identify pain. There are many misunderstandings regarding pain in animals. For example, it is thought that a dog that is not moaning or crying out is pain free. This may not be the case. Most animals are not vocal about their pain. From a survival point of view, it was to an animal’s advantage, when still wild, to suffer silently and not draw the attention of predators to themselves.
Here are a few behavioural and physical changes that could indicate pain:
- Change in normal eating habits
- It seems to hurt when you touch them
- He/she is excessively licking a joint or leg
- Your dog’s stance changed / seems abnormal
- Your dog is limping and/or walking differently
- Your dog is not that interested in playing anymore
- Lack of vocal expression OR frequent yelping/whimpering
- Walking, running, jumping and/or climbing stairs seem more difficult
- Your dog seems stiff and/or is slow to rise from his or her resting position
- Your dog’s behaviour has changed (whether it’s withdrawal, aggression, etc.)
If you notice changes in your dog’s physical appearance or behaviour, talk to your veterinarian about your concerns.
Pain Relief
Non-steroidal anti-inflammatory drugs (NSAIDs) are especially designed for animals to treat both acute and chronic pain. NSAIDs are very effective at reducing pain and stiffness and can improve the dog’s quality of life. It is important to use only pain relief medication that is prescribed by your veterinarian.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
WHAT YOU SHOULD KNOW ABOUT OSTEOARTHRITIS

Dogs and Pain
Since dogs cannot easily tell us that they are in pain and signs may be subtle, it’s difficult to identify pain. There are many misunderstandings regarding pain in animals. For example, it is thought that a dog that is not moaning or crying out is pain free. This may not be the case. Most animals are not vocal about their pain. From a survival point of view, it was to an animal’s advantage, when still wild, to suffer silently and not draw the attention of predators to themselves.
Osteoarthritis
Humans are not the only mammals that can suffer from osteoarthritis (OA). Unfortunately, dogs can develop OA too. This is a chronic disease also known as degenerative joint disease. It is considered the primary cause of chronic pain in dogs and it tends to get worse with age.
Osteoarthritis Affects a Dog’s Mobility
OA can affect one or more joints anywhere in the body; however, the most common joints affected in dogs are the hips, knees, shoulders and elbows. Most of these joints depend on a layer of cartilage acting as a cushion which also provides a smooth surface so the adjoining bones can move freely over each other.
With the onset of OA, the protective cartilage in joints wears down and this leads to painful swelling, stiffness and eventually lameness (or loss of mobility). The long-term deterioration of the cartilage is progressive and permanent.
Behavioural and Physical Changes Could Indicate Pain
Many diseases can cause behavioural changes and osteoarthritis is one of them.
Your dog may show a decreased level of activity, occasional lameness, and a stiff gait that worsens with exercise. Excessive exercise yet also inactivity, could make these symptoms worse. Cold weather may also have a negative impact. Some behavioural signs of pain may include restlessness, pacing, snapping, lethargy and decreased appetite.
If you suspect that your dog is experiencing any pain, contact your veterinarian. He or she will most likely encourage a checkup to perform tests to determine the source of the pain. Once a diagnosis is made, a treatment plan can be put in place and your dog’s comfort level and quality of life can improve.
OA can affect different joints and all dogs do not necessarily experience the same symptoms, or the same combination of symptoms.
Diagnosis
A diagnosis of OA may be done based on an assessment of historical symptoms, such as decreased activity or stiffness, as well as a physical examination which will reveal a decreased range of motion, stiff-legged gait, deformity of the joints, and swelling or pain in the joints.
No abnormal behaviour should be dismissed. Observed and documented behavioural signs could help to diagnose OA.
If it is found that your dog is affected, there are pain management medications. The right medication can help put your best friend back in motion by effectively relieving pain and inflammation.
Possible Causes of Osteoarthritis
The main cause is not clear, but many secondary causes have been identified. They include physical trauma, for example shoulder / kneecap dislocation and abnormal development / birth defects, for example elbow or hip dysplasia. Obesity should also be taken into consideration since excess weight puts additional, unnecessary stress on joints. Risks of developing OA may increase in cases where steroid treatment is prolonged or if a dog already suffers from other diseases such as, diabetes or hyperlaxity.
Pain Relief for Dogs with Osteoarthritis
Unfortunately, there is no cure, but nonsteroidal anti-inflammatory drugs (NSAIDs) can help relieve pain and improve quality of life by making the condition more manageable. Physical therapy can also be explored and some owners have turned to surgery.
If your dog is diagnosed with osteoarthritis, your veterinarian can advise you on living with and management of pain in dogs with OA. For pain relief leading to a better quality of life, scheduled check-ups and monitoring of the condition is essential.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What is Osteoarthritis?

Arthritis is a general medical term describing inflammation of the joints.
Osteoarthritis (OA) or degenerative joint disease (DJD) is the terminology used when referring to a form of chronic joint inflammation that is a progressive and permanent disease of joints. The condition can cause long-term degeneration of joints and involves cartilage tissue, bone under the cartilage, joint capsule, fluid in the joint, pain and inflammation as well as immobility.
Osteoarthritis is a very common condition in dogs and cats and it is estimated that around 30% – 50% of dogs and cats will be affected by osteoarthritis at some point in their lives.
Unlike humans this condition may manifest very early in animals due to certain underlying conditions such as hip or elbow dysplasia, broken bones and joints that are more commonly affected by wear and tear.
SYMPTOMS CAN BE MISSED
It can be easy to miss symptoms of osteoarthritis in pets because they cannot easily tell us that they are in pain and signs may be subtle. There are many misunderstandings regarding pain in animals. For example, it is thought that a dog that is not moaning or yelping is pain free. This may not be the case. Most animals are not vocal about their pain. From a survival point of view, it was to an animal’s advantage, when still wild, to suffer silently and not attract a predator’s attention.
The key symptoms of osteoarthritis are lameness, stiffness, and pain. Lameness and stiffness are evident after a period of rest or if the animal was exposed to exercise previously.
CHANGES THAT MAY INDICATE PAIN
Changes vary from pet to pet and pain can manifest in physical or behavioural changes, including:
- Reluctance to move or play. Dogs may walk more slowly, tire more easily, or refuse to play or go for walks.
- Avoid jumping. Dogs struggle to jump onto the bed and start avoiding activities that they once enjoyed.
- Difficulty with climbing or laying down. Dogs may have trouble climbing the stairs or may groan when trying to lay down.
- Limping/lameness. This is noticeable first thing in the morning.
- Pain or stiffness when getting up or down. Stiffness is particularly noticeable when pets first get up after a period of inactivity, but as the dog moves, the stiffness seems to decrease.
- Change in posture. Joint degeneration can occur in different parts of the body. Dogs may begin to hunch or stand abnormally.
- Change in personality. Pets may seem withdrawn when normally good-natured. They may seem less interested in being petted or may yelp when touched. Pain may also cause them to lose interest in eating.
With time these signs may become more obvious since the deterioration progresses and the pain worsens. Osteoarthritis in dogs is not a condition that can be cured because of the permanent deterioration of affected joints. However, there is effective pain management to bring relief and comfort. Animal-specific medications have been developed to safely deal with chronic pain in pets.
DIAGNOSIS
Diagnosing this condition can be done by firstly manipulating the joint to check for any crepitation, discomfort or pain, then followed by radiographs which are the most common tool to use and also to rule out any other conditions. Other methods of diagnosing this condition includes MRI scanning, CT scans and collection of fluid from the joint. Radiographs or X-ray tend to be the most cost effective way of diagnosing osteoarthritis.
MANAGEMENT OF OSTEOARTHRITIS
Fortunately, dogs don’t have to suffer in silence; there are several things pet owners can do to help them maintain their mobility and improve their quality of life:
- It is important to control the weight of the animal as this could have a great impact on the condition. Weight management through a prescriptive diet will also aid in weight loss in the case where the animal is overweight. More weight on joints causes more localised inflammation and irritation to the joints and this in turn can speed up the progression of osteoarthritis.
- Exercising is also a very important part of disease management. An exercise regime tailored to the animal’s specific needs can keep the joints mobile, the muscles working well and slow down the degeneration of joints.
- Comfortable surroundings such as ensuring that your pet has a warm, comfortable place to sleep that is away from drafts, can help ease pain. Provide plenty of soft bedding to help protect any painful joints. Rather than expecting your dog to negotiate stairs, provide assistance with a ramp. Help your dog to get in and out of cars.
- Non-steroidal anti-inflammatories (NSAIDs) may work very well to alleviate the pain, but it is also advisable for the pet owner to discuss with their veterinarian which ones will suit their pet the best. NSAIDs have many uses in veterinary medicine, including longer term use for treating pain associated with OA in dogs.
Contact your veterinarian for more information on the best treatment options available to manage osteoarthritis and keep your pet pain-free.
Related Articles



HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Diabetes in Cats: Symptoms

More and more cats are developing diabetes mellitus. Cat owners need to act on this alarming fact by learning more about this chronic disease.
What is Diabetes in Cats?
Diabetes is an endocrine disorder. The endocrine system features glands that produce and discharge hormones which regulate many bodily functions.
Insulin is one of these hormones. Like the human body, a cat’s body needs insulin to properly regulate blood sugar levels and to respond correctly to normal insulin levels.
Diabetes can lead to high blood sugar (hyperglycaemia) which can cause various health problems if left untreated.
Types of Diabetes in Cats
There are two types of diabetes mellitus in cats.
Type 1: Very rare in cats (but common in dogs). Essentially a decrease in the production of insulin leads to high glucose concentrations.
Type 2: The most common form of diabetes in cats. Essentially the body is unable to respond to insulin correctly, resulting in high glucose levels.
Quick FAQs and Answers About Diabetes in Cats
Is one sex more at risk?
Yes, male cats tend to be more prone to this condition.
Risk factorsfor diabetes in cats?
Age, obesity and physical inactivity.
Are certain breeds predisposed to it?
Yes, Burmese cats.
Is diabetes in cats common?
Cases are increasing and is thought to be linked with increasing levels of obesity.
Symptoms of Diabetes Mellitus in Cats
- Weight loss
- Increased thirst
- Increased appetite
- Increased urination
Other Possible Symptoms:
- Vomiting
- Poor coat
- Weakness
- Enlarged liver
- Bladder infections
- Collapse
Keep in mind that some or a combination of these symptoms can also be signs of other conditions and diseases. Either way, it’s important to bring them to your veterinarian’s attention.
So, if you’ve noticed any of these signs – even just one or two – contact your veterinarian immediately to discuss your response.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
The Management and Prevention of Diabetes in Dogs

While diabetes in dogs may not be curable, it can be managed quite successfully.
Managing Diabetes in Dogs
Here is an overview of how to manage and treat diabetes in dogs:
- Daily insulin shots given by owners at home to replace insulin
- Regular, moderate exercise that suits the affected dog’s needs
- New diet: Typically a low-fat diet high in proteins, fibre and complex carbohydrates
- Test and adjust medication/treatment: finding the correct dosage may take some time
- Monitor affected dogs at home with a daily glucose-monitoring system
- Ongoing management of diet, exercise and medication
- Going for regular veterinary check-ups
- Stay positive
Preventing Diabetes in Dogs
As a dog owner, you can prevent or reduce your dog’s risk of developing diabetes by:
- Controlling Your Dog’s Weight
Obesity contributes to insulin resistance and can increase a dog’s chances of developing pancreatitis (inflammation of the pancreas), a disease that leads to diabetes.
- Spaying Your Dog
Unspayed females are twice as likely to develop diabetes as male dogs. Spaying also helps prevent uterine infections and breast cancer (the latter of which is fatal in about 50% of dogs).
- Taking Your Dog for Routine Check-ups and in Between Visits When Necessary
Dogs can’t tell you when they feel unwell or show you exactly where it hurts. That’s why subtle physical and behavioural changes should never be ignored. So, apart from routine check-ups (typically once a year), have your dog checked out even if you’re just mildly concerned about something.
- Providing Proper Nutrition
It’s no secret that quality dog food makes a huge difference, but the problem is usually the price tag attached to it. Discuss your options with your veterinarian. Perhaps you can combine a more affordable brand with vet-approved snacks and treats, including fruits and vegetables.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
The Importance of Catching and Diagnosing Diabetes in Dogs Early

Unfortunately, there is no cure for diabetes. That’s why it’s important to notice and address the signs of diabetes in dogs early. With treatment and proper management, a healthier and longer life is possible.
What Increases the Risk of Diabetes in Dogs?
Age
Middle-aged to senior dogs (5+) are at greater risk of developing diabetes.
Sex
Unspayed females are twice as likely to develop diabetes.
Steroid Medications
Long-term use can cause diabetes.
Cushing’s Disease
Diabetes can be a complication of this disease which is caused by high levels of cortisol (stress hormone) in the blood.
Genetics
Both mixed breed dogs and purebreds are at risk. High-risk breeds include beagles, pugs, miniature poodles and -schnauzers, dachshunds and certain terriers.
Chronic or Repeated Pancreatitis
Inflammation of the pancreas can result in extensive pancreas damage which can lead to diabetes.
Obesity
Obesity is linked to acute pancreatitis and pancreatitis can lead to diabetes.
Other Health Conditions
An autoimmune disorder or viral disease could possibly be responsible for triggering diabetes in dogs.
Why is it Important to Catch Diabetes in Dogs Early?
The same rule applies to many health conditions and diseases in humans and in dogs: Early diagnosis and treatment can really promote wellness and well-being.
Here are the steps for dealing with diabetes in dogs:
- Detect it early
- Understand the condition
- Provide proper customised care
- Continue to manage it
What Can Happen When Diabetes in Dogs is Not Treated and Managed
Untreated diabetes in dogs can lead to multi-organ damage as well as:
- Seizures
- Cataracts
- Blindness
- Amputations
- Kidney failure
- Diabetic ketoacidosis(DKA): a deadly medical emergency
Act Now
Don’t wait for the severe signs and symptoms of diabetes to surface.
Contact your veterinarian if you notice any of these early signs of diabetes in dogs: excessive thirst, increased urination, weight loss and increased appetite.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Diabetes in Dogs: Symptoms

The occurrence of diabetes in canines is increasing. Find out what it is and what symptoms to watch for.
What is Diabetes in Dogs?
Diabetes is an endocrine disorder. The endocrine system features glands that produce and discharge hormones which regulate many bodily functions.
Insulin is one of these hormones. Like the human body, a dog’s body needs insulin to properly regulate blood sugar levels and to respond correctly to normal insulin levels.
Diabetes can lead to high blood sugar (hyperglycaemia) which can cause various health problems if left untreated.
Types of Diabetes in Dogs
- Diabetes Mellitus: Sugar Diabetes
Type 1: The most common type associated with a lack of insulin production.
Type 2: Inability to respond to insulin production and impaired insulin production. This type of diabetes is more common in humans.
Diabetes Insipidus: Water Diabetes
Diabetes insipidus is a very rare condition associated with excessive urination because the body fails to properly control water balance. This condition is not related to blood sugar or insulin but is rather a problem with anti-diuretic hormone (ADH).
Quick FAQs and Answers About Diabetes in Dogs
When do dogs develop diabetes?
Typically, between the ages of 4 and 14 years.
Is one sex more at risk?
Female dogs are twice as likely to develop diabetes.
Are certain breeds predisposed to it?
Possibly. It is more often seen in Miniature Schnauzers due to their risk of pancreatitis. Labrador Retrievers are also commonly affected due to their tendency to gain weight.
Is diabetes in dogs common?
Yes, diabetes mellitus type 1 is one of the most common endocrine diseases in dogs.
Are there any lifestyle/risk factors?
Yes, dogs that are overweight or obese are at higher risk of developing diabetes.
Symptoms of Diabetes Mellitus in Dogs
Since diabetes in dogs is so common, it would be wise to familiarise yourself with the signs and symptoms:
- Vomiting
- Weight loss despite having a good appetite
- Excessive thirst
- Appetite changes
- Low energy levels
- Frequent urination
- Sweet-smelling breath
- Frequent urinary tract infections
- Dehydration despite increased water intake
- The formation of cataracts
Have you noticed any of these signs? Even just one or two? Contact your veterinarian immediately to discuss the next steps.
Diabetes can be managed and dogs that are affected by it can lead long and happy lives. But it needs to be diagnosed early and treated correctly.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
An Overview of Cancer Causes and Signs in Dogs

Better health care and improved nutrition have increased the average lifespan of canines. Unfortunately, with old age comes greater cancer risks. Still, any dog can develop cancer when an abnormal growth of cells occur and stay in one part of a dog’s body or spread.
As pet owners, that’s not what we should focus on. Instead, we can familiarise ourselves with all the possible causes and signs of cancer in dogs so we can take preventative measures now and immediate action in the future if necessary.
What Can Cause Canines to Develop Cancer?
There’s no definite cause of cancer in dogs, but the following factors are believed to contribute to its development:
- Age: Dogs 10 years and older are more prone to developing cancer and sadly many do.
- Breed: Bernese Mountain Dog, Bichon Frise, Bouvier des Flandres, Boxer, German Shepherd, Golden Retriever, Great Dane, Labrador Retriever and Rottweiler.
- Sex: Some cancers can affect males more and vice versa.
- Environment: Exposure to chemicals, UV light etc.
Common Cancers in Dogs
- Skin cancers
- Bone cancer
- Blood cancers
- Canine lymphomas
- Gastrointestinal cancer
What are the Clinical Signs of Cancer in Canines?
Possible signs of cancer in dogs can include:
- Lethargy
- Vomiting
- Diarrhoea
- Weight loss
- Inappetence
- Bloody urine
- Trouble breathing
- Excessive drooling
- Difficulty urinating
- New bump or lump
- Foul-smelling breath
- Runny or bloody nose
- Wounds that aren’t healing
- Trouble eating or swallowing
- Altered features of an existing lump
- An increase in water intake and urination
- Odorous discharge from the ears
- Limping or altered gait
- Difficulty passing stools
- Stringy stool
REMEMBER: Many of the signs mentioned above are signs of other conditions and diseases as well so it’s best to consult with your veterinary health professional to get your pet thoroughly checked out.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Facts About your Cat’s Heart

FELINE CARDIOVASCULAR SYSTEM
The body needs oxygen-rich blood. The heart makes sure this blood gets around. Then, once the oxygen-depleted blood goes through the lung fields, the cycle repeats.
A cat’s heart is a small yet impressive organ which works around the clock. In fact, their little hearts beat like crazy, which is surprising, since cats seem calm and confident most of the time. OK, not literally crazy, but each human heartbeat roughly converts to three cat heartbeats.
What does the Cardiovascular System Consist of?
- A heart
- Blood Vessels: arteries, capillaries and veins
What do these components do or control?
- Blood pressure
- Control blood circulation
- Blood plasma: sugar, hormones, salts, acidity and concentration
The heart relies on messages from the nerves and hormones as well as muscle cooperation to function at its best. Despite all of these delicate and complicated processes, cats don’t get sick often, but they can still suffer from heart disease.
HEART PROBLEM SYMPTOMS
It’s not easy to tell when a cat is sick. Even signs of something more serious, for example heart problems, are often difficult to spot, if noticeable at all. Still, it helps to at least look out for the following:
- Collapse
- Weight loss
- Weakness/fatigue
- Panting and/or coughing
- Loss of or decreased appetite
- Unable or unwilling to exercise
WAYS TO PICK UP AND DIAGNOSE HEART PROBLEMS
Since a heart problem or heart disease is not obvious or even visible, you need to take your cat for regular, thorough checkups. A stethoscope won’t always cut it, but a new heart murmur could be a clue. To get answers, there are numerous tests to turn to:
- X-rays
- Hormone test
- Heartworm test
- Blood chemistry levels
- Electrocardiogram (ECG)
- Complete blood count (CBC)
- Echocardiogram: echo, 2D echo, cardiac ultrasound & echocardiography (especially 2D)
WHAT TYPES OF HEART DISEASE DO CATS GET?
Unlike dogs, cats are not often born with heart problems or malformations (congenital anomalies) and murmurs in kittens are usually harmless and short-lived.
When the heart muscle thickens, optimal pumping is compromised. In cats, this common heart disease is called hypertrophic cardiomyopathy (HCM) which can cause heart failure.
Other diseases include dilated cardiomyopathy (DCM), restrictive cardiomyopathy (RCM) and intermediate cardiomyopathy (ICM).
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Types of Rare Cancers In Cats

The following tumours and cancers are rare in cats.
BRAIN TUMOURS
Some brain tumours start in the brain. They’re called primary tumours and are very rare. Secondary tumours on the other hand develop as a result of a different cancer that has spread to the brain. Brain tumour symptoms may include:
- Seizures
- Head pressing
- Bumping into things
- Abnormal behaviour
- Meowing more; purring less
- Vision problems that affect movement
- Oversensitivity to pain or contact in the neck area
LIVER TUMOURS
Some liver tumours start in the liver, but it’s rare. Like brain tumours, liver tumours are more likely to develop due to a different cancer that has spread. Hepatocellular carcinoma is a rare but malignant tumour that affects liver tissue.
Symptoms in an advanced stage can include:
- Lethargy
- Anorexia
- Vomiting
- Diarrhoea
- Weakness
- Weight loss
- Excessive thirst
- Abdominal haemorrhage
LUNG TUMOURS
Primary lung tumours (tumours that start in the lungs) are very rare. Secondary lung cancer from tumours that metastasise (spread) are more common. Symptoms can vary greatly and may manifest in different ways.
- Fever
- Lethargy
- Vomiting
- Insomnia
- Weakness
- Loss of appetite
- Excessive hiding
- Excessive coughing
- Excessive meowing
- Laboured or rapid breathing
- Coughing up blood
- Sudden lameness
MAMMARY TUMOURS
Mammary tumours are very rare in male cats and only occasionally seen in spayed females.
Unfortunately they are very common in intact females.
NASAL TUMOURS
Unlike many brain and lung tumours, nasal tumours tend to originate in the nose and are often difficult to detect. While uncommon, nasal tumours are known to be really aggressive. Types include lymphoma (a cancer of the lymphatic system) as well as carcinoma and squamous cell carcinoma (skin cancers).
Signs and symptoms:
- Bloody nose
- Loud snoring
- Nasal discharge
- Excessive sneezing
- Rubbing or pawing at face
- Swollen or asymmetrical face
- Facial deformity
- Bulging eyes
- Seizures
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Diagnosing, Treating & Preventing Cancer in Cats

It’s important to find and treat cancer in cats as early as possible because many types of tumours in cats tend to form, grow and spread quickly. With the appropriate treatment, long-term prognosis can be improved.
DIAGNOSING CANCER IN CATS
Diagnosing cancer in cats can be complicated. Procedures and tests include:
- Urine tests
- Blood tests
- Ultrasounds: To view the size of organs and/or tumours
- Cytology: Obtain a specimen from the affected area to study the cells
- Physical Examination: Manual palpation (using hands) as well as visual observation
- X-rays (Radiography): To help identify lung, gastrointestinal tract and bladder tumours
- CT Scans: Better than X-rays for viewing possible cancer in the chest cavity, lungs and ribs
- Nuclear Medicine: Imaging technique that makes use of radioactive compounds to look for the presence and spread of cancer in the bones, kidneys, liver, lungs, spleen and thyroid
Once the veterinarian has more information, the best course of action can be recommended.
TREATING CANCER IN CATS
The recommended treatment will depend on the type and location of cancer, whether it has spread and what’s available to you.
- Surgery: Usually to remove bumps or lumps
- Chemotherapy: Drug treatment for lymphomas and aggressive tumours
- Radiation Therapy: For brain, nasal and other tumours that can’t be removed
PREVENTING CANCER IN CATS
The actual causes of cancer in cats are still unclear which makes it hard to prevent. Your best weapon is regular, thorough check-ups to ensure early detection. Also:
- Spay cats to greatly reduce the risk of mammary cancer
- Vaccinate cats to prevent the development of feline leukemia which can lead to lymphoma
If your cat has been diagnosed with cancer, talk to your veterinarian as well as a veterinary oncologist if possible to discuss all your options.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
An Overview of Cancer in Cats

It’s unclear what causes most cancers in cats. Fortunately for cat owners, feline cancer is not as common as cancer in dogs.
Still, it’s good to be aware of the signs of cancer in cats because they can hide illness which can delay diagnosis and treatment. Also, cancer in cats tends to be more aggressive so early action is imperative.
COMMON CANCERS IN CATS
- Fibrosarcoma: A soft tissue tumour
- Oral Squamous Cell Carcinomas: A malignant tumour; usually affects middle-aged to older cats
- Lymphoma: A very common malignant cancer of the lymphatic system (associated with feline leukemia virus for which there is a vaccine)
LESS COMMON CANCERS IN CATS
- Liver tumours
- Lung tumours
- Brain tumours
- Nasal tumours
- Mammary tumours (spaying has decreased incidence)
SYMPTOMS OF CANCER IN CATS
- Lumps
- Bumps
- Seizures
- Nosebleeds
- Hiding more than usual
- Discharge from eyes or nose
- Pain or discomfort in general
- Sudden weight gain or weight loss
- Loss of appetite or refusing to eat
- Skin changes including lumps and bumps
- Changes in the mouth could indicate oral cat cancer
- Breathing difficulty usually when cancer leads to fluid in the lungs
- Diarrhoea and vomiting are common with gastrointestinal lymphoma
When a cat is not thriving in general (sluggish, losing weight, poor coat conditions, etc.) he or she should see a veterinarian as soon as possible.
Related Articles
HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
10 Common Canine Cancers: Part 2

This is Part 2 of Common Canine Cancers:
Read Part 1 first.
MELANOMA
A melanoma is an aggressive, malignant tumour of melanin-forming cells associated with skin cancer. Areas that melanomas tend to target are eyes, footpads and nail beds. Tumours can also spread to organs. Possible Early Signs: Eye that drains and a swollen paw.
ORAL MELANOMA
Oral melanoma is one of the most common oral cancers seen in dogs. This type of cancer can develop anywhere around the mouth or oral cavity and spread. Dogs with dark or black colouring in their mouths are at increased risk of developing oral melanoma. A sore (inside or close to the mouth) can be an early sign of oral melanoma. Treatment Options: Surgery, radiation therapy, chemotherapy, immunotherapy or a combination.
OSTEOSARCOMA
Osteosarcoma is a type of bone cancer that’s very common in dogs. These tumours are usually malignant, grow quickly and can spread. Larger breeds aged 4 to 7 are at increased risk of developing an osteosarcoma tumour (usually in a limb). Early Signs: Lameness and swelling.
PRIMARY LUNG TUMOUR
Older dogs are more likely to develop lung cancer than younger dogs. It is often picked up by chance when X-rays are done during a check-up or other screening. A CT scan can provide more information. Pulmonary adenocarcinoma, the most common type of lung cancer in canines, causes 80% of primary lung cancer.
THYROID CARCINOMA
Older dogs are more likely to develop a thyroid tumour. It can present as a fixed or movable lump in the throat area, particularly over the windpipe covering the voice box. Signs include difficulty breathing and swallowing, weight loss and hoarseness. Treatment will depend on the affected dog’s condition.
Regular check-ups (yearly and whenever your dog is ill) are essential because early signs of cancer may be detected and diagnosed which means treatment can start sooner.
PART 1 of Common Canine Cancers features overviews of:
- Hemangiosarcoma
- Lipoma
- Lymphoma
- Mammary Gland Carcinoma
- Mast Cell Tumours
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
10 Common Canine Cancers: Part 1

Cancer is a complex disease that is unfortunately very common in both humans and dogs. It can be triggered by various things such as environmental, genetic and lifestyle factors.
Some cancers are more common than others in dogs, but dogs of all ages and breeds (crossbred or purebred) may be affected. Here are the first five in Part 1 of Common Canine Cancers:
HEMANGIOSARCOMA
Dogs are more prone to Hemangiosarcoma than any other creatures. This malignant cancer affects the cells that line the blood vessels. Areas where it typically manifests are the heart, liver, skin and spleen.
LIPOMA
Lipomas are benign, fatty tumours that grow under the skin. They’re quite common, but surgery and/or radiation is sometimes necessary. Sometimes they grow inside the chest or abdominal cavity.
Malignant lipomas are called liposarcomas which can spread.
LYMPHOMA
There are different forms of lymphoma, a cancer in the lymph nodes or bone marrow that affects the immune system. Early Signs: Swollen lymph nodes in the neck or behind knees. High-risk Age Group: 6 to 9.
MAMMARY GLAND CARCINOMA
Approximately half of mammary tumours are malignant. This cancer, which can spread, is more common in females, particularly those that are not spayed, or spayed later in life. Signs: Small nodule on/around the nipple.
MAST CELL TUMOURS
Mast cells are immune cells. Mast Cell Tumours, or mastocytomas, are the most common skin tumours in dogs. High-risk dogs include senior dogs, beagles, Boston terriers, boxers, Labradors, schnauzers and mixed breeds. Early Sign of Mastocytomas: Skin lesions. Nodules or masses can also grow inside the body.
PART 2 of Common Canine Cancers will provide an overview of:
- Melanoma
- Oral Melanoma
- Osteosarcoma
- Primary Lung Tumour
- Thyroid Carcinoma
*Source: National Canine Cancer Foundation (NCCF)
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Ear Infections in Cats: Signs, Causes, Diagnosis, Treatment & Prevention

Luckily, when it comes to ear infections, cats are not as vulnerable as dogs. Still, when they do get them, the effects can be painful and even cause damage if left untreated.
SIGNS AND SYMPTOMS OF EAR INFECTIONS IN CATS
Any or a combination of the following can indicate ear infection in cats:
- Hearing loss
- Wax buildup
- Strong odour
- Uneven pupil size (anisocoria)
- Disorientation / loss of balance
- Scratching or pawing at painful ear
- Black, dark brown or yellow discharge
- Red and/or swollen ear flap and/or ear canal
- Shaking or tilting head in direction of affected ear
- Damage/injury from scratching his or her own ears
- Discharge that resembles coffee grounds (associated with mites)
- Show of discomfort when the base of the ear is touched
- Ear canal opening featuring dark or crusty debris
COMMON CAUSES OF EAR INFECTIONS IN CATS
- Overgrowth of yeast
- Ear mites
- Allergies (food or inhalants)
- A foreign object that becomes lodged in the ear
- Overgrowth of bacteria
- Abscess caused by a bacterial infection (typically from a cat bite)
LESS COMMON CAUSES OF EAR INFECTIONS IN CATS
- Diabetes mellitus
- Ruptured eardrum
- Incorrect ear cleaning
- Autoimmune diseases
- Environmental irritants such as pollution or tobacco smoke
- Immune suppressing diseases e.g. feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV)
- Benign or malignant tumours
DIAGNOSING EAR INFECTIONS IN CATS
- Review a detailed medical history provided by the pet owner
- Complete physical exam performed by veterinarian, including examination with an otoscope
- Additional tests and procedures if needed (e.g. cytology or a culture)
TREATING EAR INFECTIONS IN CATS
Treatment will be customised to the affected cat’s need and may include:
- A liquid antibiotic for the ear
- Oral antibiotics
- Ear cleaning solutions
- Cortisone if the ear is very inflamed
- Surgery in chronic recurrent cases
PREVENTING EAR INFECTIONS IN CATS
- Keep your cat’s ears dry
- Be on the lookout for early signs of irritation
- Always consult your veterinarian if you have any concerns
- Cats that are at higher risk of developing infections should be kept indoors
IMPORTANT: DON’T TRY TO TREAT YOUR CAT’S EAR INFECTION AT HOME.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Ear Infections in Dogs: Treatment & Prevention

If your dog has an ear infection, it’s really important to approach the problem properly.
The safest and smartest first step would be to contact your veterinarian. A thorough examination may be necessary to determine the cause and severity before the appropriate treatment can be prescribed and administered.
TREATING EAR INFECTIONS IN DOGS
The first course of action would be cleaning the ears. Ideally this should be done by your veterinarian if you don’t already know how to do it. The last thing you want to do is make things worse. Your veterinarian can then provide instructions for safe home cleaning moving forward.
Topical medications (such as ointments and creams) or antibiotics are typically prescribed. Pain medication may also be necessary.
REMEMBER: It’s crucial that you don’t stray from the treatment plan. Don’t skip treatments (set reminders) and always complete the course (even if your dog appears healed). The infection might take two weeks or a month to clear, unless it’s a chronic problem that needs to be managed.
While you’re at the veterinary, ask questions such as:
How did my dog get an ear infection?
How can I reduce the risk of future ear infections?
Can ear infections be prevented completely?
PREVENTING EAR INFECTIONS IN DOGS
We all know how the saying about ‘prevention’ goes… So, before infection strikes, learn how to clean your dog’s ear correctly and safely.
- Use cotton swabs for folds, NOT for the ear canal
- Wipe the ear canal with a material that doesn’t shed fibres.
- Ask your veterinarian about cleaning solutions and how to use them if relevant
Often moisture is the culprit. So, try to keep ears dry during bath time and dry wet ears after swimming.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Ear Infections in Dogs: Signs, Causes & Diagnosis

The first thing you should know is that ear infections in dogs are quite common. The important thing is to address signs and symptoms as soon as you notice them.
SIGNS AND SYMPTOMS OF EAR INFECTION IN DOGS
- Redness
- Swelling
- Whining
- Itchiness
- Dark, stinky discharge
- Crusty or scaly ear edges
- Pawing at the affected ear
- Odours: funky or foul smelling ears
- Persistent head shaking and/or tilting
- Raw ears from scratching
DID YOU KNOW?
Symptoms = Subjective. Experienced by the affected person or animal.
Signs = Objective. Can be detected by someone other than the affected person or animal.
CAUSES OF EAR INFECTION IN DOGS
Because a dog’s ear canal has a vertical ‘L’ shape, it tends to retain fluid which can lead to health problems.
Causes of ear infection include:
- Virus
- Mites
- Injury
- Bacteria
- Moisture
- Medication
- Wax buildup
- Yeast or fungus
- Thyroid disorder
- Excessive cleaning
- Autoimmune disease
- Hormone-related disorders
- A foreign object that becomes lodged in the ear
- Allergies (allergic skin disease and food sensitivities)
- Meningitis (infected membranes around the brain and spinal cord)
- Encephalitis (inflammation of the brain)
DIAGNOSING EAR INFECTIONS IN DOGS
As with any health issues, early diagnosis is very important to ensure the problem doesn’t get worse or even dangerous. Often the goal is to prevent the infection from spreading to the middle and inner ear.
WHAT THE VETERINARIAN NEEDS TO KNOW
- Allergies or conditions
- How often ears are cleaned
- If medications were administered
- History of ear infections and details
- If you trim the hair in your dog’s ears
- Symptoms and duration of symptoms
- Foods ingested recently and in general
- Recent activities, e.g. bathing, swimming, spending time outdoors or professional grooming
VETERINARIAN EXAMINATION: POSSIBLE CHECKS AND TESTS
- Tissue culture
- Visual assessment
- Examine tissue sample
- Gentle palpation of the ear
- Examination with an otoscope
- Biopsies and X-rays (severe cases)
IMPORTANT: DON’T TRY TO TREAT YOUR DOG’S EAR INFECTION AT HOME
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
The Causes and Signs of Yeast Infection in Dogs

Yeasts are microscopic fungi. Opportunistic fungi can increase and cause skin, paw and ear infections when the circumstances are right.
The condition can be super uncomfortable and should be addressed as soon as possible before it gets worse.
Hot, humid environments are ideal for the development of yeast infections.
YEAST SKIN INFECTION IN DOGS
Yeast skin infection, also known as yeast dermatitis or Malassezia dermatitis, is an inflammatory skin condition that can affect dogs.
Simply put, Malassezia is a species of yeast that naturally occurs on the body. However, an uncontrollable overproduction of Malassezia causes problems. The yeast essentially takes over a certain area of the body, leading to skin infection.
Increased environmental humidity and temperature, a compromised immune system or strong immunosuppressive drugs are often to blame for the development of yeast skin infections.
SIGNS OF YEAST INFECTION IN DOGS
- Pain
- Licking
- Warmth
- Hair loss
- Swelling
- Redness
- Foul odour
- Greasy skin
- Hearing loss*
- Walking in circles*
- Crusty or flaky skin
- Balance problems*
- Crusts on ear flaps*
- Hair loss around ear*
- Head shaking/tilting*
- Scratching affected ear*
- Abnormal eye movements*
- Pink or red skin (early infection)
- Discharge that is yellow, bloody or brown
- Rubbing affected ear against furniture or on the floor*
- Leathery, thick and grey or black skin (chronic infection)
*Ear yeast infection specifically.
If you think your dog is suffering from a yeast infection, be sure to consult or visit your nearest veterinary.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
An Overview of Stud Tail in Cats

If you haven’t heard of stud tail in cats, or want to know more, here’s a handy overview.
WHAT IS IT?
A rare skin condition in cats found on the base of the tail.
WHAT CAUSES IT?
Stud tail is a condition caused by overactive sebaceous glands. These glands can be found at the base of the tail. They are responsible for producing waxy or oily secretions (sebum) for hair follicles to keep hair soft and flexible. When too much sebum accumulates, it leads to a buildup of foul-smelling brown material that causes this skin disease.
DID YOU KNOW?
Stud tail also goes by the following names:
- Supracaudal gland hyperplasia
- Feline tail gland hyperplasia
- Supracaudal gland infection
Stud tail mainly occurs in male cats that have not been neutered, but females and neutered males are not immune.
WHAT ARE THE SIGNS AND SYMPTOMS?
You may notice one or a combination of the following near the base of the tail:
- Pus
- Greasy fur
- Foul odour
- Red bumps
- Matted hair
- Missing hair
- Skin infection
- Waxy substance
- Light fur turning yellow
- Raw, red and/or swollen skin
- Blackheads
HOW IS IT DIAGNOSED?
Stud tail needs to be diagnosed by a veterinarian and sometimes secondary infections need to be addressed too.
HOW IS IT TREATED?
Treatment will depend on the cause and severity of the condition. Solutions include:
- Keeping the area clean / proper hygiene
- Antiseborrheic shampoo
- Antibiotics for infection
- Topical ointment
- Neutering
HOW CAN IT BE PREVENTED?
For intact males, neutering may work.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
A List of Common Skin Problems in Cats

Common problems you should be aware of:
Abscess
A painful bump filled with pus that can form after a bite or puncture wound gets infected with bacteria.
Contact Dermatitis
An allergic reaction caused by contact with particular substances or chemical irritants. A rubber or plastic allergy (from a food bowl) can manifest as itchy red bumps and inflammation.
Ear Mites
Ear mites cause great discomfort and can drive cats ‘crazy’ if left untreated. Signs include shaking or tilting the head, scratching or pawing at ears and dark brown discharge or waxy substance in the ear canal.
Feline Acne
Blackheads, sometimes caused by skin dermatitis, can occur on the edges of a cat’s lips or under the chin. Some shampoos and supplements can help.
Flea Allergy Dermatitis (FAD)
Cats that suffer from FAD are allergic to flea saliva and experience severe itching after even just one or two bites. The pimple-like bumps are typically located by the tail, rear legs and inner thighs. Proper flea control is essential.
Food Allergy Dermatitis
Certain ingredients and preservatives can cause allergic reactions in cats. Food allergies can lead to severe itching, swollen eyelids and hair loss. The head, neck and back are usually affected. Biting or scratching makes the situation worse. Sores can become infected.
Psychogenic Alopecia
A compulsive behaviour usually caused by stress. Essentially over-grooming leads to thinning of the fur.
Ringworm
Ringworm is a contagious fungal infection humans can get as well. Look for circular bald patches and a red ring or broken hairs on the head.
Stud Tail
The excretion of excessive oils (foul-smelling brown material) from glands near the tail.
Sunburn
The long-term risks associated with sunburn are skin cancers. If your cat has light-coloured fur or is a hairless breed you should take the necessary precautions.
Always contact your veterinarian if you think your cat has a skin problem.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What’s Causing Your Dog’s Skin Problems?

Nobody likes having an itchy or irritated skin and your dog is no different. Unfortunately, skin problems are very common in canines and shouldn’t be ignored. Fortunately, most causes of skin problems in dogs are not difficult to address and treat. Some can even be prevented.
Autoimmune Disorders
Blisters, hair loss, itchiness, redness, scabs and ulcers are possible symptoms of pemphigus foliaceus (autoimmune skin disease). Skin sores can also be caused by canine lupus (autoimmune disorder).
Bacterial Skin Infections
Sometimes allergies lead to additional skin problems, for example, open wounds caused by scratching, can get infected with bacteria.
Dandruff
Dry or irritated skin can lead to dandruff in dogs. Once your veterinarian has determined the cause (e.g. nutritional deficiencies or hormonal imbalances), it can be addressed.
Flea Allergy Dermatitis
Flea allergy dermatitis (FAD) is one cause of skin problems in dogs. Affected dogs are allergic to flea saliva and experience severe itching after even just one or two bites. Dogs that don’t suffer from FAD also experience itching, but not on the same level.
Environmental Allergies
An environmental allergy can be difficult to pinpoint and manage. Examples of environmental allergens include dust, mold and pollen.
Food Allergies
Food allergies can lead to itchy ears, face, paws and butt, as well as stomach problems. Common allergens include proteins, dairy and wheat.
Ringworm
Ringworm is a contagious fungal infection humans can get as well. Look for circular bald patches, rash or redness and crusty skin.
Mange
Mite infections can lead to a skin disease called mange. There are different types of mange. Signs of a mite infection include redness, hair loss, bald spots, intense itching and sores.
Yeast Infection
An increase in yeast organisms on the skin can lead to an infection, typically in moist areas (in between toes, ear canals or under arms). Symptoms include itchy skin, hair loss, redness, thickening of the skin, skin lesions and odour.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
A List of Common Eye Conditions in Canines: Part 2

6. Entropion
The term for inverted eyelids or eyelids that fold inwards is entropion. All or part of the eyelids can be affected in dogs that suffer from this painful genetic condition. The abnormality causes the eye’s surface to become irritated from hair or lashes scratching it. Later, damage can lead to corneal ulceration, perforation or the buildup of dark scar tissue. Watch out for excessive tearing and squinting.
7. Glaucoma
Basically when eye fluids are unable to drain, eye pressure increases. Symptoms include cloudy corneas, dilated pupils, pain, increased tearing, redness and sometimes enlarged eyes. Untreated glaucoma usually results in impaired vision and eventually blindness.
8. Keratoconjunctivitis Sicca (KCS) or Dry Eye
Adequate ‘tears’ are required to keep eyes lubricated. A deficiency in the aqueous tear film in dogs is responsible for dry eye (‘syndrome’), or keratoconjunctivitis sicca (KCS). The disorder is characterised by severely dry eye surfaces and dry eyelid linings. Symptoms vary, so any concerns should be reported to your veterinarian.
9. Lens Luxation
Lens luxation is the official term for a dislocated eye lens (the eye lens ‘leaves’ its allocated area). Dogs older than three and younger than 10 are typically affected. Breeds that are prone to lens luxation include border collies, cocker spaniels, German shepherds and terriers.
10. Progressive Retinal Atrophy (PRA)
Progressive retinal atrophy (PRA) is another genetic disease that causes blindness and unfortunately it’s not easy to catch. Essentially the ‘film’ (retina) is wrinkled or scarred. The first warning sign: Night vision issues.
THAT’S IT FOR PART 2!
Find out more about the following conditions in Part 1:
- Cataracts
- Cherry Eye
- Blepharospasm
- Conjunctivitis (Pink Eye)
- Corneal and Scleral Wounds
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
A List of Common Eye Conditions in Canines: Part 1

Dogs’ eyes are very important organs that help them form images of the world. Threats to healthy eyes include injuries, conditions and diseases.
The following are considered common eye conditions in canines:
1. Blepharospasm
Blepharospasm means involuntary blinking or twitching of the eyelids. Rather than a condition or disease, blepharospasm is a clinical indicator of an eye-related problem. Signs and symptoms of blepharospasm include red, swollen and/or itchy eyelid(s); spasmodic blinking; scratching or rubbing of the face or eyelids; eye discharge; crusty or flaky eyelid skin; and pimple-like bumps.
2. Cataracts
The eye lens is the transparent structure behind the pupil. Cataracts cause the eye lens to appear cloudy or bluish-gray. The condition can cause pressure and vision problems, including blindness.
3. Cherry Eye
Dogs have one hidden and two visible eyelids. The concealed one hides in your dog’s inner eye corner. Ligaments keep it in place but an inherited weakness can cause it to ‘pop’ out. Cherry eye requires treatment.
4. Conjunctivitis (Pink Eye)
The conjunctiva is a mucous membrane found inside the eyelids. When it becomes inflamed we call it conjunctivitis, or pink eye. There are several causes. Signs include blepharospasm (see above), redness, eye discharge and swelling.
5. Corneal and Scleral Wounds
The eye’s outer, clear tissue (that sits in front of the iris and pupil) is called the cornea. The white outer layer of the eyeball is called the sclera. Both are delicate and certain objects or incidents can cause corneal or scleral abrasion. Types of wounds include cuts, punctures and ulcers. A red, watery eye is often a sign of injury.
THAT’S IT FOR PART 1!
Find out more about the following conditions in Part 2:
- Entropion
- Glaucoma
- Keratoconjunctivitis Sicca (Dry eye)
- Lens Luxation
- Progressive Retinal Atrophy (PRA)
If you think your dog might have an eye condition, be sure to consult your veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
A List of Common Eye Conditions in Felines

Cats have very unique and beautiful eyes. They can detect much more light than we can, however, their colour vision is limited. Threats to healthy eyes include injuries, conditions and diseases.
The following are considered common eye conditions or problems in felines:
- Allergies/Irritants
This is a tricky one since symptoms are very similar to other conditions and problems. So, if you notice redness or discharge (especially if it doesn’t go away or gets worse) visit a veterinary.
- Cataracts
The eye lens is the typically transparent structure in the centre of the eye behind the pupil. Cataracts, that cause the lens to appear milky white or cloudy gray, can result in vision problems, including blindness.
- Corneal Ulcers
The eye’s clear surface tissue is called the cornea which admits light into the eye. Open sores in this area are called corneal ulcers. Causes include injury, infection, tear production issues or other abnormalities. Signs and symptoms include cloudy cornea, pain, squinting, redness and in some cases discharge.
- Discolouration of the Iris
Iris melanosis manifests as brown ‘freckles’ on the coloured rim of tissue around the pupil typically in cats around 7 years and older. When a dark pigment appears on the iris it can be a sign of iris melanoma (a type of cancer).
- Glaucoma
Glaucoma in cats is an emergency. When eye fluids are unable to drain, eye pressure increases. Affected cats are usually in pain and can lose their vision and even their eyes. There are many causes. Signs and symptoms include cloudy, red, weepy and sometimes enlarged eyes.
- Infections
Causes: bacteria, fungi, parasites and viruses. Possible signs and symptoms: discharge, redness, swelling, rubbing, squinting, sneezing and nasal discharge.
- Trauma
Physical injury (a cut, puncture or scratch) can be caused by accidents, fights and materials getting stuck in the eye. Signs and symptoms: redness, swelling, pain, discharge and visible damage.
Other diseases include:
- Conjunctivitis (pink eye)
- Dendritic corneal ulcers
- Nasolacrimal duct obstruction (NLDO)
- Uveitis
If you think your cat might have an eye condition or injury, visit a veterinarian.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
CAT ANXIETY

OVERVIEW
As in humans, stress and anxiety in cats can impair the ability to function and further aggravate existing physical conditions.
ENVIRONMENTAL CAUSES OF ANXIETY IN CATS
Any change in a cat’s environment can cause stress and anxiety. Environmental changes are often the cause and emotional stress is the effect.
A CHANGE IN YOUR CAT’S ROUTINE
Cats prefer predictability. Any change in a daily routine should be handled by planning ahead and acclimatising your cat to the change.
MOVING RESIDENCE
Moving is a major disruption and calls for care and putting in measures so that your cat’s routine is disrupted as little as possible. Create a ‘safe room’ filled with your cat’s belongings in a quiet corner in the new residence.
NEW HOUSEHOLD MEMBER
Introducing a new member of the household to your cat requires care and patience. It’s best that the new member allows the cat to approach rather than forcing the interaction.
VETERINARY VISITS
Most cats are frightened of veterinary visits. Placing your cat in a crate covered by a light blanket may help in reducing your cat’s anxiety.
LOUD NOISES
Cats react adversely to loud and abrupt noises. When we as humans get startled by sounds, we can figure out that the noise won’t harm us, unlike cats.
FRUSTRATION AT INABILITY TO DEFEND TERRITORY
When your cat suddenly sees a strange cat and is frustrated because it can’t get outside to defend the territory, it could attack the closest being, whether it is another resident pet or an unsuspecting human.
SEPARATION ANXIETY
If your cat has a history of abandonment or prior neglect, it may display anxious behaviour, such as licking and biting at itself.
HOW TO MANAGE ANXIETY IN CATS
The first step is to determine the stress or fear trigger that is causing anxiety in your cat. Once you have established the cause, take measures to manage your cat’s anxiety. Once you have eliminated the stressor, your cat’s anxiety will be eased. What may appear insignificant to you, such as providing a new litter box, closing the window shades, or toning down loud music in your home, can make a major difference in decreasing your cat’s stress levels.
Your cat can also detect and react to your personal stress so it’s most important that you keep your own stress level down to help alleviate your cat’s fears and anxieties.
If you’re unable to find the stressor, a visit to your veterinarian is in order. Your veterinarian will examine your cat to rule out other conditions that might be causing your cat’s behaviour, such as thyroid disease.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
STRESS IN DOGS

OVERVIEW
Dogs, like humans, can experience chronic stress causing a variety of physical issues that can develop into serious health problems.
Prolonged stress may also affect a dog’s emotional state making him more aggressive or potentially dangerous. Stress or anxiety are more common in dogs than we think. Dogs can’t verbalise their stress, worry or anxiety, but they do communicate their emotional state through body language and behaviour.
To avoid dogs becoming chronically stressed, it is important to notice the signs of stress at an early stage and introduce intervention tactics as soon as possible.
SIGNS OF STRESS IN DOGS
There are many different signs of anxiety; some are subtle while others are not. Recognising these signs is the first step in creating a safe, comfortable space for a dog. It’s important to consider what could be triggering the stress.
The main signs that a dog has anxiety include:
- Changes in general behaviour
- Cowering behaviour or a desire to hide
- Loss of interest in things like walks and treats
- Decrease in appetite
- Destructive behaviour
- Urination in the house or other inappropriate bathroom behaviour
- Excessive barking or crying
- Anxiety as you get ready to leave
- Excessive panting
- Shaking or tucked-in tails
- Trying to escape
- Diarrhoea, constipation or other digestive issues
- Licking and biting himself
- Aggression toward people or other animals
- Excessive drooling or shedding
- Excessive pacing
- Increased sleeping
Because these can be generalised symptoms, diagnosing anxiety in your dog can be a challenge. It’s important to take note of the situation and context when these behaviours arise and recognise triggers that can be causing these problems.
This information will help your veterinarian when diagnosing the underlying issues of the stress.
CAUSES
There is no one single cause for anxiety in dogs. Each dog is unique and reacts differently to the external environment.
Main contributors to dog anxiety include:
- Separation Anxiety: This is triggered when the dog becomes fearful and upset as soon as he is separated from his guardians.
- Noise Anxiety: Fear of and the corresponding stress responses to loud noises. This may be triggered by noises, such as fireworks, thunderstorms, vacuum or even bird noises. Noise anxiety can tie in to phobias.
- Phobias: An external trigger or situation that causes an intense and persistent fear. Common phobias include: strangers, children, other animals, being restricted, hats, sunglasses and car rides.
- Pain or illness: If a dog has a health condition and is in pain, he may develop some form of fear or anxiety associated with an external trigger.
- Age: An elderly dog that is experiencing changes within his nervous system may react fearfully to an external situation.
- Traumatic Experiences: In unfamiliar situations or new surroundings dogs can become fearful and anxious, especially if they have experienced trauma earlier in life.
- Deprived Early in Life: If a dog has not been socialised or has been contained in a confined space without environmental exposure, he may develop anxiety as well.
HOW TO HELP EASE ANXIETY IN DOGS
Every dog is unique. What works for one dog may not work for another, and it often takes some experimentation to figure out what plan of action will work best for your dog.
Some dogs learn to manage their phobias through behaviour modification alone. Others may need the help of drug therapies, like anti-anxiety medication.
Your veterinarian will be able to recommend the appropriate treatment plan.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
EAR INFECTIONS IN CATS

OVERVIEW
Ear infections, causing painful itchiness and irritation, are not as common in cats as they are in dogs.
Although ear infections themselves are problematic, there can be underlying causes of the inflammation of the external ear canals that become inflamed.
If your cat gets an ear infection, it should be addressed immediately to minimise pain and damage to the ear canal.
SIGNS OF EAR INFECTION IN CATS
Symptoms may vary a great deal, depending on the severity of the ear infection.
The following are some signs that indicate an infection:
- Scratching to the point of damaging skin
- Scabs, dark or crusty debris in the ear canal opening
- Pain when the ears are massaged
- Head tilt or inability to keep balance
- Uneven pupil size
CAUSES
The main causes of ear infections in cats are:
- An abscess from a bite wound or scratch
- Ear mites (parasite)—especially in kittens; highly contagious among cats
- Allergies
- Growth in the ear canal
DIAGNOSIS
Depending on the underlying cause, ear infections can resolve quickly or develop into a chronic condition. Your veterinarian will take a thorough history of your cat to determine if an underlying disease may be the cause. Your cat will be given a complete physical exam, including the use of an otoscope to look down the ear canal. Other tests or procedures may be performed for an accurate diagnosis.
Some additional tests your veterinarian may recommend include:
- Cytology, which identifies if yeast, bacteria, or other microorganisms are present
- A culture to determine which type of bacteria is present
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
CHRONIC EAR INFECTIONS IN DOGS

OVERVIEW
Ear infections, causing painful itchiness and irritation, are one of the most common problems afflicting dogs.
Although ear infections themselves are problematic, there are usually underlying causes of the inflammation of the external ear canals that become inflamed with bacterial or yeast overgrowth. With overgrowth of these organisms, inflammation of the ear canal increases causing swelling and narrowing the tubes. Inflammation also causes an increase in the wax production. External ear infections may progress to involve the middle and inner ear, leading to more serious signs of disease.
Chronic infection can permanently damage the ear canal and cause pain, neurologic signs, and deafness.
SIGNS OF EAR INFECTION IN DOGS
Symptoms may vary a great deal, depending on the severity of the ear infection.
External ear infections may progress to involve the middle and inner ear, leading to more serious signs of disease:
- External ear infection (otitis externa)
- Painful, itchy sensitive ears
- Cry or groan
- Rubbing or scratching at ears
- Shake their heads
- Discharge, redness and odour from the ears
- Scabs or crusting on the inside of the outer ear
- Narrowing or even closing of the canals
- Middle ear infection (otitis media)
- Pain when opening mouth or reluctance to chew
- Paralysis of the nerves in the face
- Dry eye
- Hearing loss
- Abnormal pupil size
- Inner ear infection (otitis interna)
- Inability to keep balance, stand, or walk
- Nausea or vomiting
- Head tilting/shaking
- Walking in circles
CAUSES
While bacteria are associated with ear infections, your veterinarian will determine the reason for your dog’s discomfort and if there is a certain disorder or disease that is the primary reason that the ear infections develop.
These conditions include:
- Foreign objects in the ear
- Trauma to the body, such as head injuries
- Ear mites increasing the likelihood of bacterial infection
- A specific strain of yeast (Malassezia) that can lead to infection
- A fungus (Aspergillus) linked to ear infections and inflammation
- Conformation: Large floppy ears cover the canal, trap moisture and decrease airflow creating the perfect environment for bacteria and yeast
- Allergies
- Hypothyroidism can lead to a variety of different side-effects, including dry skin, bacterial infections and subsequent chronic ear infections
- Polyps or tumours in the ear canal
DIAGNOSIS
Depending on the underlying cause, ear infections can resolve quickly or develop into a chronic condition. Your veterinarian will perform a complete physical exam of your dog, including the use of an otoscope to look down the ear canal. Other tests or procedures may be performed for an accurate diagnosis.
Some additional tests your veterinarian may recommend include:
- Cytology, which identifies if yeast, bacteria, or other microorganisms are present
- A culture to determine which type of bacteria is present
- Blood tests to rule out hypothyroidism, autoimmune disease, or other underlying problems
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Pain Management For Your Dog

Like humans, dogs are happier when they are healthy and pain-free. The thing is, it’s not always obvious when a dog is experiencing discomfort. It’s up to dog owners to learn about signs and symptoms of pain so it can be managed.
CAUSES OF PAIN
Pain can be caused by infections, injuries and diseases. With ageing also comes certain degenerative changes in the body.
Conditions and illnesses that can cause pain:
- Ear infection
- Gum disease
- Cystitis: bladder inflammation
- Slipped disc: a common cause of paralysis
- Pancreatitis: inflammation of the pancreas
- Osteoarthritis (OA): also known as degenerative joint disease
- Peritonitis: Inflammation of the tissue that lines the inner wall of the abdomen
- Cancer: common tumours in dogs include lymphoma, haemangiosarcoma, mast cell tumours and osteosarcoma (bone cancer)
HOW TO KNOW IF YOUR DOG IS EXPERIENCING PAIN
Certain symptoms could be signs that your dog is experiencing pain. Ask yourself, ‘Is my dog…’
- Vomiting
- Vocalising
- Experiencing diarrhoea
- Having trouble sleeping
- Not eating or eating less
- Sluggish or unresponsive
- Limping or moving strangely
- Continuously licking the same spot
- Flattening her or his ears against their head
- Seeking more than the usual amount of attention
- Acting aggressively (growling, biting or snapping)
- Whining, whimpering or howling for no (obvious) reason
- Behaving differently: hiding, antisocial, unenthusiastic or restless
WHAT TO DO IF YOU THINK YOUR DOG IS EXPERIENCING PAIN
If you suspect that your dog is in any pain there are two things you should do. The first is to stay calm while you assess the situation. The second is to taken action, while remaining calm and sensible.
Whether you think it’s serious or not, many experts agree that you should contact a veterinarian immediately. You will most likely have to take your dog for a check-up. Don’t waste time guessing or trying to find solutions on your own.
Sometimes the cause of pain can be diagnosed. In cases where it cannot, pain medication could be administered to manage the pain in the meantime.
DO NOT GIVE YOUR DOG HUMAN MEDICINE
Pain Management Options
Nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to reduce and manage pain in dogs. A veterinarian will have to perform a physical examination and other tests if necessary to determine which medications would be most effective for the situation and your dog’s health. Make sure you get verbal and written instructions on how to administer medication and ask about possible side effects.
Behavioural changes, loss of appetite, skin problems (redness or scabs) and digestive issues (tarry stool, diarrhoea and vomiting) could indicate a negative reaction to medications/NSAIDs. Phone your veterinarian if you notice symptoms associated with your dog’s medication.
NSAIDs can help with stiffness, joint pain and swelling. For example, with the right treatment plan, dogs with osteoarthritis can enjoy a better quality of life.
There are cases where other medications need to be considered, but this will be discussed with you if and when necessary. Supplements are also available but it’s not always clear how effective they are.
Not all forms of pain can be resolved, but proper management can make a big difference in your dog’s life.
NOTE: Do not use dog medications for a dog other than the canine patient it was prescribed for.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Constipation In Cats

OVERVIEW
Constipation is the inability to routinely and easily evacuate the bowels resulting in retention of faeces or passage of hard, dry faeces.
When a cat is constipated, the colon – the section of the lower intestine that contains undigested food, mucus, bacteria, and dead cells before elimination – has become impacted with faeces that will not move.
Occasional constipation can generally be treated with dietary changes, enemas, and medication.
If the condition is left untreated, it can develop into obstipation – the severe, end-stage form of this disease process. At this point the colon is enlarged, blocked up or ‘impacted’. The cat may require hospitalisation and therapy, such as manual removal under anaesthetics of hardened faecal matter.
Megacolon is a condition in which the colon becomes grossly dilated, muscle tone is lost and it is unable to expel faecal material. Megacolon leads to severe constipation and could be life threatening. Treatment usually involves surgery to remove sections of the colon.
With advanced constipation the cat is completely unable to evacuate its bowels. The colon is so enlarged and stretched that the barrier that normally prevents bacteria from moving from the cat’s faeces into its bloodstream is no longer functioning. With translocation of bacteria, the cat becomes systematically ill and will die, if left untreated.
SYMPTOMS
Constipation can affect cats at any age, but is seen more frequently in older cats.
Constipation or obstipation may exhibit the following signs:
- Straining to defecate with little or no production of faeces
- Because of pain, constipated cats may vocalise during attempts at defecation
- Infrequent or no defecation
- Hard, dry faeces possibly with some blood or mucus on the surface
- Defecating outside the litterbox
- Small quantities of faeces
- Small amount of liquid stool with mucus or blood
- Decreased appetite and thirst
- Vomiting
- Lethargy
CAUSES
Some potential causes of constipation and obstipation include:
- Inappropriate diet
- Traumatic injury
- Blockages from foreign materials or hairballs
- Stress in the home
- Reluctance to use the litterbox because of a change in litter – a dirty box
- Lack of exercise
- Decreased water intake
- Painful urination
- Dehydration, often caused by kidney disease
- Nerve damage
- Arthritis, making it painful to squat
- Tumours
- Some drugs, including anaesthetics
- Underlying metabolic abnormality
DIAGNOSIS
Following a physical exam and discussion of your cat’s symptoms, tests may include:
- Baseline blood tests
- A blood chemistry analysis
- Urinalysis
- Abdominal palpation – the veterinarian’s hands probe the abdominal area along the entire length of the colon to see if it is distended with faecal matter
- Radiographs (X-rays) to confirm suspected constipation and show the extent to which the colon is dilated and whether a narrowing appears to be present
- Ultrasound imaging to rule out the presence of an obstructive tumour
- Endoscopic exam (inserting a tube containing a small camera into the rectum) done under anaesthesia. This enables the veterinarian to check for abnormalities such as narrowing of the colon or tumours
- A biopsy of the tissue may also help identify other disease processes
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Constipation In Dogs

OVERVIEW
Constipation is the inability to routinely and easily evacuate the bowels resulting in retention of faeces or passage of hard, dry faeces.
When a dog is constipated, the colon – the section of the lower intestine that contains undigested food, mucus, bacteria, and dead cells before elimination – has become impacted with faeces that will not move.
Occasional constipation can generally be treated with dietary changes, enemas, and medication.
If the condition is left untreated, it can develop into obstipation – the severe, end-stage form of this disease process. At this point the colon is enlarged, blocked up or ‘impacted’. The dog may require hospitalisation and therapy, such as manual removal under anaesthetics of hardened faecal matter.
Megacolon is a condition in which the colon becomes grossly dilated, muscle tone is lost and it is unable to expel faecal material.
Megacolon leads to severe constipation and could be life threatening. Treatment usually involves surgery to remove sections of the colon.
With advanced constipation the dog is completely unable to evacuate its bowels. The colon is so enlarged and stretched that the barrier that normally prevents bacteria from moving from the dog’s faeces into its bloodstream is no longer functioning.
With translocation of bacteria, the dog becomes systemically ill and will die, if left untreated.
SYMPTOMS
Constipation can affect dogs at any age, but is seen more frequently in older dogs.
Constipation or obstipation may exhibit the following signs:
- Straining to defecate with little or no production of faeces
- Because of pain, constipated dogs may vocalise during attempts at defecation
- Infrequent or no defecation
- Hard, dry faeces
- Pain or yelping when eliminating
- Small quantities of faeces
- Small amount of liquid stool with mucus or blood
- Decreased appetite and thirst
- Occasional vomiting
- Poor appetite
- Lethargy
- Swelling around the anus
CAUSES
Some potential causes of constipation and obstipation include:
- Dehydration
- Inappropriate diet
- Traumatic injury
- Blockages from foreign materials such as bones or hair
- Lack of exercise
- Poor diet
- Decreased water intake
- Painful urination
- Dehydration, often caused by kidney disease
- Nerve damage
- Arthritis, making it painful to squat
- Tumours
- Some drugs, including anaesthetics
- Underlying metabolic abnormality
- Change of home environment
DIAGNOSIS
Following a physical exam and discussion of your dog’s symptoms, tests may include:
- Baseline blood tests
- A blood chemistry analysis
- Urinalysis
- Tests for signs of arthritis, which could account for your dog’s reluctance to posture
- Radiographs (X-rays) to confirm suspected constipation and show the extent to which the colon is dilated and whether a narrowing appears to be present
- Ultrasound imaging to rule out the presence of an obstructive tumour
- Colonoscopy (inserting a tube containing a small camera into the colon) done under anaesthesia. This enables the veterinarian to check for abnormalities such as narrowing of the colon, rectal lesion or tumours
- A biopsy of the tissue may also help identify other disease processes
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Abscesses in Dogs

OVERVIEW
A common skin condition in dogs is an abscess that can form if an irritation worsens or if bacteria invades the skin.
An abscess can be quite unsightly and alarming and can be found on almost any part of a dog’s body.
Whether small or large, abscesses will often cause redness, if visible under the skin. In some instances, an abscess will burst, discharging an unpleasant-smelling secretion or may cause local tissue damage. Surface wounds are quite common but if they become infected and are left untreated your dog may experience other complications.
An abscess can also be located inside a body cavity or deep within tissue.
Abscesses can lead to serious conditions and when the abscess is located inside the body – in the liver, for example – there may be fever and the additional complication of a disseminated internal infection or bacteria in the bloodstream, if the abscess is ruptured internally.
A dental abscess can also form under a dog’s tooth and have the potential to develop into a systemic bacterial infection, which can be life-threatening.
SYMPTOMS
Signs of an abscess include:
- Pain displayed by pawing at the abscess or limping
- Pus, blood or fluid from the area
- Red, inflamed or swollen skin
- A small scab with redness or warmth in the surrounding skin
- Loss of hair over the area
- Excessive itching, licking or nibbling at the area
- Loss of energy or appetite
- Bad breath
- Swelling of the face or bleeding gums
- Round, visible bump in the mouth
- Excessive drooling
- Fever
- Lethargy
DIAGNOSIS
Your veterinarian will give your dog an initial physical exam and take a bacterial culture or swab test of the infected area to determine the strain of bacteria present.
A blood test will also be performed to see if the infection has migrated to the bloodstream. In the case of dental abscesses, an x-ray will be taken to determine the severity of the abscess.
Early diagnosis and treatment of abscesses, whether external or internal, can help avoid progression of disease.
TREATMENT
The prognosis for most abscesses is generally good with immediate treatment.
A skin abscess treatment usually involves cleansing, draining and flushing the wound followed by topical solutions and ointments and an antibiotic regimen, if required. In the case of dental abscesses, a root canal, extraction, or saving the affected tooth will be recommended. A course of antibiotics is usually prescribed for both skin and dental abscesses to ensure the infection is completely wiped out. To help ease your dog’s suffering, your veterinarian may also prescribe pain medication.
If the bacteria has gone deep into the tissue or is located inside the body or has infected the blood, alternative treatment options will be considered.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Abscesses in Cats

OVERVIEW
A common skin condition in cats is an abscess that can form if an irritation worsens or if bacteria invades the skin.
An abscess can be quite unsightly and alarming and can be found on almost any part of a cat’s body.
Whether small or large, abscesses will often cause redness, if visible under the skin. In some instances, an abscess will burst, discharging an unpleasant-smelling secretion or may cause local tissue damage. Surface wounds are quite common but if they become infected and are left untreated your cat may experience other complications.
An abscess can also be located inside a body cavity or deep within tissue.
Abscesses can lead to serious conditions and when the abscess is located inside the body – in the liver, for example – there may be fever and the additional complication of a disseminated internal infection or bacteria in the bloodstream, if the abscess is ruptured internally.
A dental abscess can also form under a cat’s tooth and have the potential to develop into a systemic bacterial infection, which can be life-threatening.
SYMPTOMS
Signs of an abscess include:
- Pain displayed by pawing at the abscess or limping
- Pus, blood or fluid from the area
- Red, inflamed or swollen skin
- A small scab with redness or warmth in the surrounding skin
- Loss of hair over the area
- Excessive itching, licking or nibbling at the area
- Loss of energy or appetite
- Bad breath
- Swelling of the face or bleeding gums
- Round, visible bump in the mouth
- Excessive drooling
- Fever
- Lethargy
DIAGNOSIS
Your veterinarian will give your cat an initial physical exam and take a bacterial culture or swab test of the infected area to determine the strain of bacteria present.
A blood test will also be performed to see if the infection has migrated to the bloodstream. In the case of dental abscesses, an x-ray will be taken to determine the severity of the abscess.
Early diagnosis and treatment of abscesses, whether external or internal, can help avoid progression of disease.
TREATMENT
The prognosis for most abscesses is generally good with immediate treatment.
A skin abscess treatment usually involves cleansing, draining and flushing the wound followed by topical solutions and ointments and an antibiotic regimen, if required. In the case of dental abscesses, a root canal, extraction, or saving the affected tooth will be recommended. A course of antibiotics is usually prescribed for both skin and dental abscesses to ensure the infection is completely wiped out.
If the bacteria has gone deep into the tissue or is located inside the body or has infected the blood, alternative treatment options will be considered.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Acid or Gastroesophageal Reflux (GERD) in Cats

OVERVIEW
Cats, like humans, can suffer from acid or gastroesophageal reflux disease, GERD. Acid reflux is quite common in cats and while younger cats are at greater risk, cats of all ages may be susceptible.
During a gastric reflux episode there is an uncontrollable reverse flow of gastric or intestinal fluids into the tube connecting the throat and the stomach (esophagus). Gastric fluids are strongly acidic, almost colourless liquids secreted by the glands in the lining of the stomach and are necessary for digestion.
These stomach acids can cause damage to the protective mucus lining of the esophagus resulting in inflammation.
SYMPTOMS
Usually experienced after meals, acid reflux can cause a degree of damage to the esophageal lining.
A mild inflammation of the esophageal lining is referred to as mild esophagitis, while more severe esophagitis causes damage (ulceration) to the deeper layers of the esophagus. A common symptom is if your cat regurgitates undigested food, mucus or fluid.
Your cat may experience pain (meowing, howling, etc.) while swallowing, lack of appetite and weight loss. Other symptoms may include uncontrolled gulping and salivation or coughing. With severe esophagitis fever and excessive salivation may be present.
CAUSES
Gastric reflux may occur because of poor positioning during an anaesthetic procedure that causes the opening between the stomach and the esophagus (sphincter) to relax.
Failure to fast before anaesthesia can also result in gastroesophageal reflux. Congenital hiatal hernia and cancers of the esophagus are some of the medical conditions that can increase your cat’s risk of acquiring gastric reflux. Long-term or chronic vomiting also increases the likelihood of gastric reflux.
DIAGNOSIS
Aside from a routine examination, your veterinarian will perform an esophagoscopy, and examination which uses an internal camera to view the lining of the esophagus.
This procedure checks your cat’s esophageal lining for bleeding or an irregular surface in the mucus lining. Your veterinarian will then determine if the changes in the mucus of the esophagus are consistent with esophagitis as a result of gastroesophageal reflux.
Other diagnoses include swallowing of a caustic agent, a foreign body or tumor in the esophagus, a hiatal hernia, or disease of the mouth or throat.
TREATMENT
Dietary changes are advisable and the primary treatment options.
Your veterinarian may recommend withholding food for one to two days to allow your cat’s esophagus to heal. Following this, a dietary regimen of low-protein, low-fat diet served in frequent small meals can be introduced. This diet is effective since fat decreases the strength of the muscle between the stomach and esophagus and proteins stimulate the release of gastric acid.
Your veterinarian may also prescribe medication to strengthen the gastroesophageal sphincter and improve digestion.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Acid or Gastroesophageal Reflux (GERD) in Dogs

OVERVIEW
Dogs, like humans, can suffer from acid or gastroesophageal reflux disease, GERD. Acid reflux is quite common in dogs and while puppies are at greater risk, dogs of all ages may be susceptible.
During a gastric reflux episode there is an uncontrollable reverse flow of gastric or intestinal fluids into the tube connecting the throat and the stomach (esophagus). Gastric fluids are strongly acidic, almost colourless liquids secreted by the glands in the lining of the stomach and are necessary for digestion.
These stomach acids can cause damage to the protective mucus lining of the esophagus resulting in inflammation of the esophagus (esophagitis).
SYMPTOMS
Usually experienced after meals, acid reflux can cause a degree of damage to the esophageal lining.
A mild inflammation of the esophageal lining is referred to as mild esophagitis, while more severe esophagitis causes damage (ulceration) to the deeper layers of the esophagus. A common symptom is if your dog regurgitates undigested food, mucus or fluid.
Your dog may experience pain (yelping, howling, etc.) while swallowing, a lack of appetite and weight loss. Other symptoms may include uncontrolled gulping and salivation or coughing. With severe esophagitis fever and excessive salivation may be present.
CAUSES
Gastric reflux may occur because of poor positioning during an anaesthetic procedure that causes the opening between the stomach and the esophagus (sphincter) to relax.
Failure to fast before anaesthesia can also result in gastroesophageal reflux. Congenital (present at birth) hiatal hernia and cancers of the esophagus are some of the medical conditions that can increase your dog’s risk of acquiring gastric reflux. Long-term or chronic vomiting also increases the likelihood of gastric reflux.
DIAGNOSIS
Aside from a routine examination, your veterinarian will perform an esophagoscopy, an examination which uses an internal camera to view the lining of the esophagus.
This procedure checks your dog’s esophageal lining for active bleeding or an irregular surface in the mucus lining. Your veterinarian will then determine if the changes in the mucus of the esophagus are consistent with esophagitis as a result of gastroesophageal reflux.
Other diagnoses include swallowing of a caustic agent, a foreign body or tumour in the esophagus, a hiatal hernia, or disease of the mouth or throat.
TREATMENT
Dietary changes are advisable and the primary treatment options.
Your veterinarian may recommend withholding food for one to two days to allow your dog’s esophagus to heal. Following this, a dietary regimen of low-protein, low-fat diet served in frequent small meals can be introduced. This diet is effective since fat decreases the strength of the muscle between the stomach and esophagus and proteins stimulate the release of gastric acid.
Your veterinarian may also prescribe medication to strengthen the gastroesophageal sphincter and improve digestion.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Acute Diarrhoea in Cats

OVERVIEW
Cats with acute diarrhoea may defecate more frequently, and may have softer, looser or more watery faeces. Blood, mucus, or even parasites may be visible in or on their stools and they may have accidents in the house.
Diarrhoea is quite common and is brought on by a wide range of causes. Most cases of diarrhoea resolve in a few hours or days, but ensure that your cat has plenty of fresh water available to avoid dehydration. Very old cats and kittens, which are more susceptible to dehydration, or those already suffering from some other medical problem, should be seen by the veterinarian more quickly.
Often diarrhoea will resolve on its own. However, if your cat continues to suffer from loose stools and other symptoms for more than a day, take him to your veterinarian immediately.
If there is also vomiting, lethargy or loss of appetite, the diarrhoea is indicative of more serious causes.
SYMPTOMS
Diarrhoea is characterised by stool that is soft, loose or watery.
Other signs may include:
- Straining during bowel movement
- Accidents in the house
- Mucus or blood in the stools
- Worms in the stools
- Defecating more often
These signs may indicate a more serious problem and your cat should be seen by your veterinarian without delay:
- Fever
- Pain/discomfort
- Loss of appetite
- Weight loss
- Weakness or tiredness
- Abdominal pain
- Nausea or vomiting
- Lethargy/depression
- Blood in the stool (black, tar-like stool or visible, red blood)
CAUSES
There are many reasons for your cat to have loose stools.
Here are some general causes:
- Dietary change – change of diet or ingesting foreign objects, such as, bones, string and toys
- Infections – viral or bacterial infections
- Parasites – e.g. roundworms and hookworms irritate gastrointestinal tract
- Stress – anxiety or excitement can result in gastrointestinal upset
- Drugs and toxins – some medications can upset the gastrointestinal tract and certain toxins can also cause diarrhoea
- Inflammatory disorders – inflammatory bowel disorders can cause your cat to develop diarrhoea
- Metabolic diseases – thyroid imbalances or diseases in other organs, such as the liver or pancreas can upset the environment in the gastrointestinal tract resulting in diarrhoea
- Cancer
WHEN IS DIARRHOEA IN CATS AN EMERGENCY?
It’s important to assess your cat. If he seems to be happy and playful and isn’t displaying other symptoms, such as weakness, decreased appetite, vomiting and if the diarrhoea resolves itself over a period of a day, it’s probably not an emergency situation.
If your cat’s diarrhoea is prolonged and accompanied by a significant change in behaviour and an onset of other alarming symptoms, you should consider this an emergency and take him to the veterinarian immediately.
DIAGNOSIS
The veterinarian will perform a thorough history and physical exam to determine possible causes of the diarrhoea. Faecal examinations, blood tests and X-rays may also be needed. Advanced testing, if required, may include ultrasound or intestinal biopsy.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Acute diarrhoea in Dogs

OVERVIEW
Dogs with acute diarrhoea may defecate more frequently, and may have softer, looser or more watery faeces. Blood, mucus, or even parasites may be visible in or on their stools and they may have accidents in the house.
Diarrhoea is quite common and is brought on by a wide range of causes. Most cases of diarrhoea resolve in a few hours or days but ensure that your dog has plenty of fresh water available to avoid dehydration. Very old dogs and puppies, which are more susceptible to dehydration, or those already suffering from some other medical problem, should be seen by the veterinarian more quickly.
Often diarrhoea will resolve on its own. However, if your dog continues to suffer from loose stools and other symptoms for more than a day, take him to your veterinarian immediately.
If there is also vomiting, lethargy or loss of appetite, the diarrhoea is indicative of more serious causes.
SYMPTOMS
Diarrhoea is characterised by stool that is soft, loose or watery.
Other signs may include:
- Straining during bowel movement
- Accidents in the house
- Mucus or blood in the stools
- Worms in the stools
- Defecating more often
These signs may indicate a more serious problem and your dog should be seen by your veterinarian without delay:
- Fever
- Pain/discomfort
- Loss of appetite
- Weight loss
- Weakness or tiredness
- Abdominal pain
- Nausea or vomiting
- Lethargy/depression
- Blood in the stool (black, tar-like stool or visible, red blood)
CAUSES
There are many reasons for your dog to have loose stools.
Here are some general causes:
- Dietary change – change of diet or ingesting foreign objects, such as, bones, string and toys
- Infections – viral or bacterial infections
- Parasites – e.g. roundworms and hookworms irritate gastrointestinal tract
- Stress – anxiety or excitement can result in gastrointestinal upset
- Drugs and toxins – some medications can upset the gastrointestinal tract and certain toxins can also cause diarrhoea
- Inflammatory disorders – inflammatory bowel disorders can cause your dog to develop diarrhoea
- Metabolic diseases – thyroid imbalances or diseases in other organs, such as the liver or pancreas can upset the environment in the gastrointestinal tract resulting in diarrhoea
- Cancer
WHEN IS DIARRHOEA IN DOGS AN EMERGENCY?
Is diarrhoea important to assess your dog? If he seems to be happy and playful and isn’t displaying other symptoms, such as weakness, decreased appetite, vomiting and if the diarrhoea resolves itself over a period of a day, it’s probably not an emergency situation.
If your dog’s diarrhoea is prolonged and accompanied by a significant change in behaviour and an onset of other alarming symptoms, you should consider this an emergency and take him to the veterinarian immediately.
DIAGNOSIS
The veterinarian will perform a thorough history and physical exam to determine possible causes of the diarrhoea. Faecal examinations, blood tests and X-rays may also be needed. Advanced testing, if required, may include ultrasound or intestinal biopsy.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Diabetes in Dogs

OVERVIEW
Diabetes, or diabetes mellitus in dogs, is a chronic disease caused when the body cannot properly respond to the hormone insulin, which is produced and release by the pancreas.
As in the human body, the cells in a dog’s body need energy in the form of glucose (sugar) for their metabolism and other functions. Glucose in the blood needs insulin to ‘unlock’ the door to cells. Insulin attaches to cells and signals when the time is right to absorb glucose.
By absorbing glucose, cells in the liver, the muscles and fat deposits get energy for their functioning while glucose levels in the blood are regulated.
If your dog isn’t producing enough or any insulin, the cells in his body are unable to absorb glucose from the blood and they become starved of energy.
In Type I diabetes, glucose concentrations are high because the pancreas doesn’t make enough insulin.
In the case of Type II diabetes, glucose levels are high because cells in the body are unable to effectively use available insulin, or when the pancreas is producing some insulin, but not enough for the body’s needs.
Most diabetic dogs have Type II diabetes and many of them require insulin to adequately control their illness. If too much glucose builds up in the dog’s body due to the lack of insulin, the disease can become dangerous and even life threatening.
SYMPTOMS
Depending on the stage of disease, clinical signs can include the following:
- Increased thirst
- Dehydration
- Urinating more than usual
- Increase or decrease in appetite
- Weight loss, even with increased food intake
- Tiredness
- Vision loss
- Vomiting
- Loss of back leg control
CAUSES
The exact cause of diabetes in dogs is difficult to identify. However, diabetes seems to affect overweight dogs, because obesity makes the dog’s body less responsive to the effects of insulin.
Older dogs are also more susceptible to diabetes. Diseases like hyperthyroidism and chronic pancreatitis may also make dogs more prone to develop diabetes.
DIAGNOSIS
If a dog presents any suspicious clinical signs, such as increased drinking, your veterinarian will perform a thorough physical examination and recommend tests to check glucose concentrations in the blood and urine.
These tests may include:
- CBC (complete blood count) and chemistry profile: These initial blood tests provide information about the dog’s organ systems. They may show dehydration, an elevated blood sugar level, or other changes that can occur with diabetes.
- Urinalysis: Evaluation of a urine sample may show the presence of sugar (glucose) in the urine if diabetes is present.
- Fructosamine test: Fructosamine is a protein in the blood that binds very securely to glucose. This provides a long-term view of blood glucose over the previous one to three weeks. In a dog with diabetes, the blood sugar levels are likely high for long periods of time.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Diabetes in Cats

OVERVIEW
Feline diabetes, or diabetes mellitus, is a disease caused when the body cannot properly respond to the hormone insulin, which is produced and released by the pancreas.
As in the human body, the cells in a cat’s body need energy in the form of glucose (sugar) for their metabolism and other functions. Glucose in the blood needs insulin to ‘unlock’ the door to cells. Insulin attaches to cells and signals when the time is right to absorb glucose.
By absorbing glucose, cells in the liver, the muscles and fat deposits get energy for their functioning while glucose levels in the blood are regulated.
If your cat isn’t producing enough or any insulin, the cells in his body are unable to absorb glucose from the blood and they become starved of energy.
In Type I diabetes, glucose concentrations are high because the pancreas doesn’t make enough insulin.
In the case of Type II diabetes, glucose levels are high because cells in the body are unable to effectively use available insulin, or when the pancreas is producing some insulin, but not enough for the body’s needs.
Most diabetic cats have Type II diabetes and many of them require insulin to adequately control their illness.
If too much glucose builds up in the cat’s body due to the lack of insulin, the disease can become dangerous and even life threatening.
SYMPTOMS
Depending on the stage of disease, clinical signs can include the following:
- Increased thirst
- Dehydration
- Urinating more than usual
- Increase or decrease in appetite
- Weight loss, even with increased food intake
- Tiredness
- Vision loss
- Vomiting
- Weakness in the back of legs
CAUSES
The exact cause of feline diabetes is difficult to identify. However, diabetes seems to affect overweight cats, because obesity makes the cat’s body less responsive to the effects of insulin.
Older cats are also more susceptible to diabetes. Diseases like hyperthyroidism and chronic pancreatitis may also make cats more prone to develop diabetes.
DIAGNOSIS
If a cat presents any suspicious clinical signs, such as increased drinking, your veterinarian will perform a thorough physical examination and recommend tests to check glucose concentrations in the blood and urine.
These test may include:
- CBC (complete blood count) and chemistry profile: These initial blood tests provide information about the cat’s organ systems. They may show dehydration, an elevated blood sugar level, or other changes that can occur with diabetes.
- Urinalysis: Evaluation of a urine sample may show the presence of sugar (glucose) in the urine if diabetes is present.
- Fructosamine test: Fructosamine is a protein in the blood that binds very securely to glucose. This provides a long-term view of blood glucose over the previous one to three weeks. In a cat with diabetes, the blood sugar levels are likely high for long periods of time.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
A Heart-to-Heart About Pet Heart Health

If you love your pets with all your heart it’s important to know more about their hearts and what may happen to this vital organ during the course of their lives.
HEART DISEASE IN PETS
Heart disease is common in both cats and dogs.
Heart disease in cats is often asymptomatic, that is, no signs or symptoms are showing.
Many affected dogs may remain asymptomatic, but some may develop complications that could end in congestive heart failure.
In dogs, heart disease is either present from birth (congenital) or acquired during their lifetime. In approximately 95% of the cases heart disease in dogs is acquired and 5% of the cases reported are congenital heart disease.
TYPES OF HEART DISEASE AND ASSOCIATED CAUSES
Congenital conditions are mostly the result of genes. Sometimes it’s a defect; other times it can be a hereditary (inherited) condition. You also don’t know when a defect can start causing problems.
Acquired conditions could be caused by injury, infection (parvo) or normal wear and tear (age). Different breeds are prone to different diseases.
HEART DISEASE PREVENTION
The following measures may all help fight the onset of heart disease, delay it or help with recovery and management of the disease:
- A healthy diet which is balanced and nutritious
- Frequent exercise appropriate for size and age
- A happy life that includes ample affection and appropriate discipline
One way to prevent certain heart diseases in pets is to give your pets quality parasite prevention as often as required. Correct dosage and administration is very important in terms of safety and efficiency.
Sadly not all types of heart disease can be prevented. Still, investing in the wellbeing of your pets (physically, emotionally and financially) and providing them with a stress-free environment is important no matter what the situation.
Although old age is inevitable, there is a lot that can be done in conjunction with your veterinarian to give your pet happy, healthy golden years. Old age is not a disease, but it does predispose your pet to many diseases for example heart disease. Working closely with your veterinarian will help detect symptoms prematurely and institute treatment promptly. Make sure you take your senior pets for annual wellness checks, particularly if they are a breed prone to heart disease.
You could consider taking out pet insurance while your pets are still healthy to make treatment and management of the condition more accessible and affordable should you need it.
SIGNS ASSOCIATED WITH HEART CONDITIONS IN DOGS:
- Respiratory problems can be related to heart disease, for example; coughing, shortness of breath and/or laboured breathing. Bluish gums could indicate low blood oxygen.
- If your dog is behaving strangely or seems unhappy he or she could be suffering from a heart disease. This can include restlessness and weakness.
- Weight problems, mostly weight loss, is another warning sign, especially if no dietary changes have been made.
- A swollen belly should alarm you too.
- If the disease continues to progress it could result in hind limb paralysis and sudden death.
SIGNS ASSOCIATED WITH HEART CONDITIONS IN CATS:
- Vomiting
- General weakness
- Respiratory problems
- Fainting and/or collapsing
- Decreased/lack of appetite
- Grey or bluish gums or tongue
- Thromboembolism (obstruction of blood vessel by blood clot dislodged from another site in the circulation)
- Depression/antisocial behaviour
- Weight loss, weight gain and/or swollen belly
- If the disease continues to progress it could result in hind limb paralysis and sudden death
DIAGNOSIS
Apart from routine check-ups and vaccinations, please discuss any health or behavioural concerns with a veterinarian.
He or she will know which questions to ask and which exams and/or screenings to perform.
TREATMENT
There is no one-size-fits-all medication for heart diseases and conditions.
For example, some treatments are only for dogs with clinical evidence of heart failure, and are used to increase the ability of the heart to pump blood. Other dogs or cats may require blood thinners, blood pressure medications or just basic supplements.
Your veterinarian should guide you and elaborate on how to manage your pet’s condition. It’s extremely important to follow instructions and to stay consistent with treatments. You may have to monitor and change certain aspects of your pet’s routine as well.
Related Articles
Facts About a Dogs Heart Read Now
Heart Disease In Dogs Read Now
What You Need To Know About Heart Attacks In Dogs Read Now
Congestive Heart Failure (CHF) As a Result Of Dilated Cardiomyopathy (DCM) Read Now
Congestive Heart Failure (CHF) As a Result Of Atrioventricular Valvular Insufficiency (AVVI) Read Now







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Vaccinate against Kennel Cough

WHAT IS KENNEL COUGH?
Kennel Cough is an infectious respiratory disease of dogs which usually results in a persistent, dry hacking cough.
Usually found in environments where there has been recent contact with a single or group of infected dogs. The pathogens are then spread in the air through coughing or sneezing.
It can be used by a number of different pathogens, but the most frequent culprits are:
- Bordetella bronchiseptica (bacteria)
- Canine parainfluenza (virus)
- Canine Adenovirus (type)
WHAT DIFFERENTIAL DIAGNOSIS SHOULD THE VETERINARIAN ALSO CONSIDER?

AIM OF VACCINATION
Won’t necessarily prevent the animal from getting the infection, but to reduce the chance of them developing clinical signs of this disease complex.
Speak to your veterinarian about vaccinating your pets against KENNEL COUGH.
Related Articles


HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Aspiration (or Inhalation) Pneumonia in Dogs

Dog owners need to be aware of the risk of aspiration (or inhalation) pneumonia.
WHAT IS ASPIRATION (OR INHALATION) PNEUMONIA?
Aspiration pneumonia, also called inhalation pneumonia, occurs when a dog’s lungs become inflamed due to the aspiration (or inhalation) of a foreign substance, including vomit, food, foreign bodies and regurgitated gastric acid.
This leads to a bacterial infection in the respiratory tract. This usually occurs after a dog vomits and inhales a portion of the regurgitated material.
The seriousness of the condition depends on the bacteria that are present in the inhaled material, and the distribution of the aspirated material into the lungs.
If the pneumonia is severe enough to restrict the flow of oxygen, aspiration pneumonia can be life-threatening.
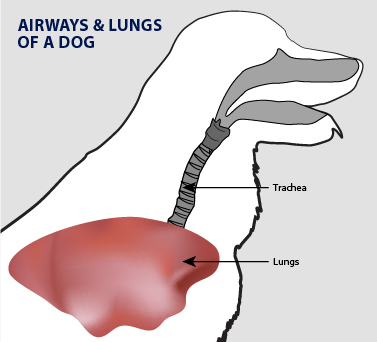
CAUSES OF ASPIRATION PNEUMONIA
It’s not the actual vomiting that causes aspiration pneumonia. It’s the bringing up of contents from the stomach that are then inhaled. Inhalation of foreign matter, from vomiting or from the regurgitation of gastric acid contents can be problematic.
Inhalation of smoke, kerosene, mineral oil, gasoline, or other caustic chemicals can also cause problems.
Neuromuscular disorders, which would cause difficulty with swallowing, can also result in aspiration pneumonia.
A common cause of aspiration pneumonia is faulty administration of liquid medication. Any liquid that’s given via syringe, whether medication or food, must not be given any faster than the animal can swallow, or there is a risk of aspiration pneumonia.
DOGS AT RISK OF ASPIRATION PNEUMONIA
Dogs that develop aspiration pneumonia typically have a history of:
- Vomiting
- Recent anaesthesia
- Neurologic problems
- An underlying medical condition that predisposes the dog toward aspiration
Medical conditions that make a dog more likely to inhale matter that has been vomited into their lungs include:
- Laryngeal paralysis
- Megaesophagus
- Persistent right aortic arch (seen in puppies)
- Congenital oesophagus problems
- Gastrointestinal disease
Dogs that are forced-fed have a higher risk. Puppies are also at risk of aspiration pneumonia, especially if they’re bottle-fed.
SYMPTOMS OF ASPIRATION PNEUMONIA
Aspiration pneumonia may include:
- Loss of appetite
- Regurgitation
- Vomiting
- Coughing
- Fever
- Lethargy
- An altered mood
- Breathing difficulties
- Swallowing difficulties
- Panting
- An increased heart rate
- Exercise intolerance due to weakness
- Open mouth breathing
- Noisy or wet breathing
- Discharge from nasal passages
- Blue-coloured gums
- A bluish tinge to the skin (cyanosis)
- Stretching of the neck out to breath
- Collapse
Related Article
Upper Respiratory Infections In Cats Read Now







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What you need to know about heart attacks in dogs

The heart muscle is called the myocardium. An infarction is the obstruction of the blood supply to an organ or region of tissue. Myocardial infarction, which literally means ‘heart tissue damage or death’, is the medical term for a heart attack that is deadly and needs immediate medical attention.
When blood – which transports oxygen and nutrients – is unable to reach a certain part of the heart muscle, tissue damage and tissue death occur, preventing the affected part to effectively pump blood throughout the body.
Fortunately canine heart attacks are rare, however, risks rise when heart disease, certain genetic factors or abnormalities from birth are present.
CAUSES OF CANINE HEART ATTACK
- Tumour(s): When a tumour grows on or around the heart vasculature (blood vessels), it can block blood flow to the heart muscle
- Hypothyroidism: When the thyroid gland fails to produce thyroxine hormone which turns food into fuel for the body
- Nephrotic Syndrome: Kidney disease which results in kidney damage can lead to loss of protein that helps prevent blood clots from forming which can cause canine heart attack
- Bacterial infection: Blood flow to the heart muscle can be hindered due to inflammation and blockage caused by infection
- Vasculitis: Inflammation of blood vessels can be caused by infection, immune-mediated disease or other injury to endothelial linings
- Atherosclerosis: It’s rare in dogs, but plaque buildup can restrict blood flow and even lead to artery rupture
- Coronary artery disease: Although also very rare in dogs, damage or disease in the heart’s major blood vessels can happen with severe hypothyroidism and associated with high serum cholesterol levels
HEART ATTACK SYMPTOMS
Not all dogs have the same symptoms and there’s little or no warning before it can happen. The following symptoms are associated with canine heart attack:
- Seizure
- Rigidity
- Collapse
- Head tilt
- Lethargy
- Vomiting
- Weakness
- Lameness
- Immobility
- Confusion/anxiety
- Slight fever (over 39.4 °Celsius)
- Panting, abnormal breathing or breathing problems
- Increased heart rate (large breeds: 100+ beats p/min; small breeds: 140+ beats p/min)
- Sudden death
Heart disease in pets may lead to fainting (syncope) which can be confused for a heart attack, but it doesn’t necessarily cause permanent damage.
DIAGNOSING CANINE HEART ATTACK
In order for a veterinarian to make a diagnosis, a dog owner will need to provide the veterinarian with a detailed description of the signs and symptoms observed, along with a comprehensive health history. A physical examination, with a focus on the cardiovascular system, will also need to take place. Tests, which can help to determine the cause of the heart attack, include:
- Check thyroid gland function
- Check kidney and metabolic function with urinalysis
- Check for infection with complete blood count (CBC)
- Check kidney and liver function with biochemistry and blood culture
- Chest X-ray: View heart size and check for fluid around the heart and possible masses
- Electrocardiography (ECG): Review cardiac electrical impulses and measures arrhythmias
- Echocardiography: Check for fluid or masses around the heart, examine heart valve function, heart muscle and pericardial health
TIP: Ask your veterinarian about a holter monitor/ambulatory ECG for monitoring heart health at home.
WHAT TO DO WHEN YOU THINK YOUR DOG IS HAVING A HEART ATTACK
- Stay calm and contact a veterinarian immediately.
- Keep other pets and children away from your dog.
- Food or water intake could be dangerous so rather prevent it.
- Minimise or eliminate stimuli because it could contribute to panic.
- To comfort your dog, you can wrap him/her in a blanket if it’s not a hot day.
- CPR is not recommended, unless you’re professionally trained and know it’s necessary.
- You can attempt to record heart rate to determine if it improves. Ask your veterinarian how.
- Safely and comfortably transport your dog to the veterinary if he or she collapses.
TREATMENT AND RECOVERY PLAN
There are various courses of action to consider. The best option will depend on the affected dog and severity of the heart attack. One or a combination of the following could be recommended to regain and maintain normal heart activity:
- Resuscitation
- Supportive care
- Diet improvements
- Pacemaker implants
- Adjustment in activity
- Surgery (if there’s a mass)
- Antiarrhythmic medications
- Hospitalisation (to monitor heart)
- Thyroid replacement medications
- Antibiotics for infection or inflammation
- Preventative or supportive care for renal conditions
- Blood thinners (to improve circulation)
- Other medications
Accurate diagnosis and appropriate treatment can help dogs live long, happy lives after a heart attack.
RECOVERY AND HEALTH MANAGEMENT POST HEART ATTACK
The recovery will depend on how serious the heart attack was (extent and duration), what caused it and how the cause(s) can be treated. For some causes, treatment may have to continue for the rest of the dog’s life. Regular check-ups, tests and monitoring may also be necessary. The pet owner could benefit from learning how to check vital signs at home.
OTHER SERIOUS HEART CONDITIONS
About 10% of all dogs suffer from heart disease. Mitral valve disease (MVD) is the most common form of heart disease in dogs and dilated cardiomyopathy (DCM) is the second most common form of heart disease in dogs.
For more information about heart conditions in dogs, visit our conditions and diseases section.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
HEART DISEASE IN DOGS

It’s terrible to think about it, but pets can also suffer from heart problems. Congenital heart disease (heart disease that’s been there from birth) is usually picked up in puppies and is not that common. Acquired heart disease, which develops during the course of a dog’s life, accounts for most heart conditions.
Both can lead to congestive heart failure (CHF), because the heart is struggling to pump blood to the whole body. Acquired heart disease is caused by:
- Atrioventricular valvular insufficiency (AVVI), a valvular disease also known as mitral valve disease or endocardiosis, is the most common cause of canine CHF.
- Dilated cardiomyopathy (DCM) is the second most common cause of canine CHF.
AVVI
As this degenerative disease becomes worse, heart valve leaflets are damaged. This means the valves can’t close properly and blood leaks backward into the atrium, eventually causing a heart murmur. Cardiac function and circulation are then hindered.
DCM
With this disease the heart muscle becomes weak and large, preventing it from pumping blood efficiently. This causes decreased cardiac output and tissue perfusion.
When it comes to diagnosing CHF, it’s crucial that detection happens early and quick treatment follows. The problem, however, is that the clinical signs and symptoms can be similar to respiratory disease.
COMMON CLINICAL SIGNS OF AVVI OR DCM:
In the early stages, signs are usually subclinical (symptoms are not obvious yet). This phase can last months or years. AVVI progresses slowly, but DCM can have a quick onset and progresses rapidly. Both eventually lead to congestive heart failure. As either progress, common clinical signs may include:
- Coughing
- Weakness and fainting
- Poor appetite and weight loss
- Restlessness, usually at night
- Difficulty exercising (easy to tire; reluctant to go for walks)
- Behavioural changes (lack of energy; depressed; withdrawn)
- Difficulty breathing; shortness of breath; increased respiratory rate
HOW TO CORRECTLY IDENTIFY CHF WITH SPECIFIC DIAGNOSTIC TOOLS
- Clinical History (assess age, breed and history in terms of behaviour, breathing, appetite, etc.)
- Physical Examination (examine weight and body condition, pulse abnormalities, etc.)
- Cardiac and Pulmonary Auscultation (to detect a heart murmur caused by blood leakage )
- Thoracic Radiographs (for info about heart size, changes in the lungs, etc.)
- Additional Diagnostic Tests (blood- & urine tests, echocardiography, electrocardiograms, etc.)
Once you notice signs of heart disease, you should consult your veterinarian as soon as possible so that diagnostic tools can provide answers. Unfortunately there is no cure for CHF, but therapeutic intervention can improve symptoms and prolong life.
Related Articles
Facts About a Dogs Heart Read Now
A Heart-to-heart about Pet heart health Read Now
What You Need To Know About Heart Attacks In Dogs Read Now
Congestive Heart Failure (CHF) As a Result Of Dilated Cardiomyopathy (DCM) Read Now
Congestive Heart Failure (CHF) As a Result Of Atrioventricular Valvular Insufficiency (AVVI) Read Now

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Pancreatic Cancer (Adenocarcinoma) in Dogs

WHAT IS PANCREATIC CANCER (ADENOCARCINOMA) IN DOGS?
The pancreas is a gland organ in the digestive and endocrine systems. It is responsible for hormonal and digestive functions.
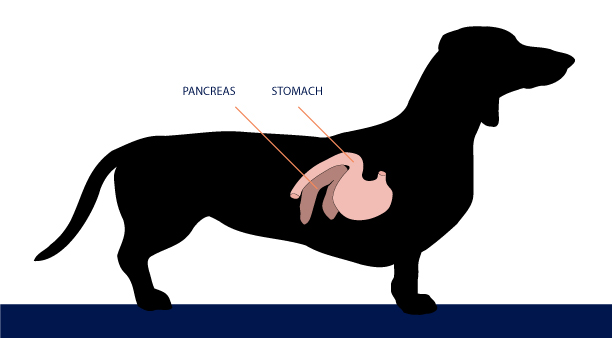
Pancreatic cancer develops as abnormal pancreatic cells multiply rapidly in the pancreas. These cells don’t die, but continue growing to form tumours, which in time, can result in the death of the normal surrounding pancreatic tissue.
Canine pancreatic cancer is rare but the cancerous tumours (adenocarcinomas) are aggressive and malignant. Like other carcinomas it grows rapidly and metastasizes to other parts and organs of the body. In most dogs metastasis is found at the time of diagnosis, thus making treatment difficult for these patients.
RISK FACTORS OF PANCREATIC CANCER IN DOGS
Similar to other types of cancer, adenocarcinoma of the pancreas usually affects older dogs (eight years or older). It can occur in any breed or gender of dog, but older female dogs and Airedale terriers, Spaniels, and Boxers tend to be more susceptible to this disease.
The underlying cause of pancreatic cancer in dogs is not clear.
SYMPTOMS OF PANCREATIC CANCER IN DOGS
Canine pancreatic cancer often doesn’t cause symptoms until the disease reaches its later stages. Many symptoms of pancreatic cancer in dogs are non-specific.
A dog with pancreatic cancer may show signs such as:
- Weakness
- Appetite loss
- Weight loss
- Seizures
- Lethargy
- Vomiting
- Abdominal distension
- Abdominal pain
- Hyperglycaemia (elevated blood sugar level) or hypoglycaemia (low blood sugar levels)
- Ascites (fluid accumulation in the peritoneal cavity)
- Jaundice (yellowing of the skin, eyes and mucous membranes)
In extreme cases, signs of pancreatic insufficiency (inability to digest food properly due to a lack of digestive enzymes produced by the pancreas) may also be shown.
In the later stages of pancreatic cancer, dogs may experience a range of other symptoms, depending on what part of their body is affected by the spread of cancer.
There is no curative treatment for this tumour. Surgery and medications are used in those cases in which treatment is suggested. A partial or total surgical removal of the pancreas may be performed in theory but overall the prognosis is grave.
Fortunately this type of cancer is quite rare in dogs.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Stomach and Intestinal Cancer (Leiomyosarcoma) in Cats

WHAT IS STOMACH AND INTESTINAL CANCER (LEIOMYOSARCOMA) IN CATS?
Stomach and intestinal cancer is also known as leiomyosarcoma, which arises from the smooth muscles of the stomach and intestines.
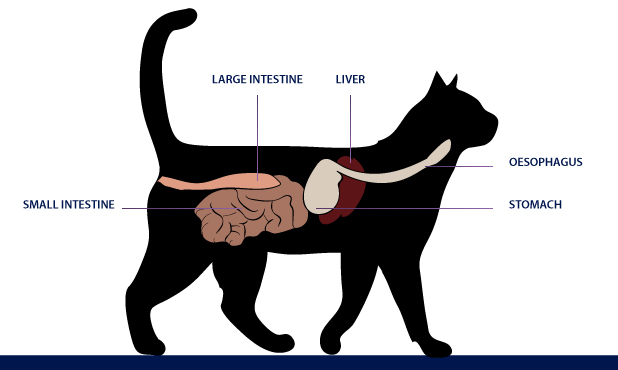
Leiomyosarcoma is an uncommon cancerous tumour that is an extremely serious and painful disease.
This cancer has a tendency to metastasize (or spread) to other areas in the gastrointestinal tract and other body organs.
RISK FACTORS FOR LEIOMYOSARCOMA
This cancer affects mostly older cats (older than six years). All breeds are equally susceptible to leiomyosarcoma.
SYMPTOMS OF LEIOMYOSARCOMA
Leiomyosarcoma in cats is a silent killer because it often goes undetected.
A cat with stomach cancer rarely shows symptoms and therefore, its diagnosis and treatment are difficult.
Some of the signs of this cancer are also symptoms of common stomach disorders, which makes diagnosis even more difficult.
Most symptoms are related to the gastrointestinal tract and may include:
- Vomiting
- Loss of appetite
- Lethargy and weakness
- Diarrhoea
- Weight loss
- Breathing problems
- Frequent stomach problems
- Blood in stool
- Gas
- Growling or rumbling sounds in stomach
- Feeling of incomplete defecation
- Weight loss
- Limping
If your cat is showing any of the above symptoms, your veterinarian will first take a full history. Be sure to provide as much information as possible to aid in the diagnosis. They will then conduct a full medical examination. In many cases, further tests will be required to rule out other more common causes of the above-mentioned symptoms. The vet will generally start with blood tests and often x-rays and ultrasound examinations will be needed. To make a definitive diagnosis of leiomyosarcoma, the vet may need to do surgery to get a biopsy of the stomach wall.
Treatment usually depends on the stage of cancer. When surgery is indicated, it usually involves removal of the tumour mass along with some normal tissue.
Post-operative pain and inflammation following biopsy or surgery can be reduced.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
At Home Management for Cats with CKD

Once a cat has been diagnosed with Chronic Kidney Disease (CKD), a few things need to happen.
AS THE OWNER OF A CAT WITH CKD, YOU NEED TO:
- Understand what it means and deal with the news, emotionally.
- Work out a treatment plan with your veterinarian to manage your cat’s CKD.
- Stick with the treatment plan to ensure the best outcome for as long as reasonably possible.
- Follow up with your veterinarian as often as required to ensure the treatment plan is still appropriate.
- Accept (and prepare for) the fact that CKD cannot be cured.
THE POINT OF MANAGING CKD AT HOME
Unless underlying conditions or symptoms are severe, cats with CKD are generally not hospitalised. It’s up to owners to take care of their cats.
WHAT CAT OWNERS SHOULD AIM TO ACHIEVE WHEN MANAGING THEIR CAT’S CKD AT HOME
- Maximum time – Help your cat live a longer life with the disease.
- Optimum wellness – Help your cat feel as good as possible while living with the disease.
WAYS TO MANAGE CKD AT HOME
WATER
Dehydration is one of the big problems associated with CKD. This entails ensuring that there is always enough, easily accessible, clean water for your cat to drink every day. A drinking fountain could be considered. It may also help to add extra water to the cat’s food if a wet diet is not followed.
NUTRITION
Cats with CKD require similar diet changes, but each cat should follow a customised treatment plan based on his or her body’s needs during the different stages of the condition. Some cat foods have been designed with CKD in mind to help prevent ongoing kidney damage or the build-up of excess waste products in the blood. Blood and urine tests enable the monitoring of vitamins and minerals to guide dietary adjustments and other necessary treatments.
ENVIRONMENT
Sick pets, like sick people, fare better in safe, comfortable environments where they can relax and rest as often as needed. In a house where other pets and children are present, stress and noise should be minimised if possible. Preferably more than one clean, comfy and quiet sleeping area should be offered to allow this. This affected cat should also be kept safe from natural elements.
MEDICATION
Just like some cat foods have been designed with CKD in mind, certain medications have been produced to help combat some of the effects of CKD, such as significant amounts of protein lost in urine and blood pressure. Other medications may also be necessary for managing underlying conditions. Talk to your veterinarian about your options so that treatment can start as soon as possible to improve the outcome.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
10 Tips for Cat Owners caring for a cat with CKD

Stay positive – for the sake of your cat – and your sanity.
Finding out that your cat has Chronic Kidney Disease (CKD) is usually devastating, but there’s hope yet. Armed with positive attitude and a customised treatment plan provided by your veterinarian, it’s often possible to enjoy many more happy years together.
FAMILIARISE YOURSELF WITH THE DISEASE
Information is power, so be sure to get answers to the following questions:
- What is CKD? Get as many facts as possible to understand the disease.
- What are the stages of CKD? Learn how stages are classified and what happens during each one.
- What does having CKD mean for my cat? Ask your veterinarian to explain how the disease will develop and what you need to expect and prepare for.
FIND OUT WHAT YOUR CAT’S SPECIFIC NEEDS ARE
Several factors will determine the needs of a cat with CKD. These include:
- THE CAUSE OF CATS WITH CKD: Are there underlying factors or is it unknown? If present, underlying conditions should be addressed and treated along with clinical signs.
- TEST RESULTS: Have certain vitamin, mineral or hormone imbalances been discovered? These need to be addressed and monitored moving forward.
- HEALTH PROBLEMS: Does your cat have an infection or inflammation? It’s a common complication so the possibility needs to be ruled out or confirmed and treated.
STAY ON TOP OF HYDRATION
Getting dehydrated is very dangerous in general and it’s much worse for cats with CKD. Therefore, keep asking yourself the question: Is my cat drinking enough water? If not, your veterinarian should be able to provide advice on how you can increase intake.
MAKE SURE YOUR CAT IS EATING ENOUGH
Questions to answer:
- Since being diagnosed, has your cat’s diet been adapted? It’s usually necessary.
- If yes, is your cat eating enough of his or her new food? It’s essential.
- Do you need help getting your cat to eat enough? Speak to your veterinarian for further assistance.
Weight loss should always be a cause for concern and even more so in cats with CKD.
REMAIN ALERT AND TREAT SYMPTOMS WHEN THEY ARISE
Report symptoms, as you notice them, to your veterinarian. After a check-up and perhaps some tests, he or she will likely prescribe medication to help your cat feel better. Things you may notice include vomiting, diarrhoea and lethargy.
DON’T STRAY FROM THE TREATMENT PLAN, BUT MAKE SURE IT’S ADAPTED WHEN NECESSARY
To help ensure the best outcome for the remainder of your cat’s life (which may well be a couple of years), it’s important to remain consistent with regards to treatment. That means don’t skip check-ups and don’t forget to give your cat’s medication as instructed.
ASK YOUR VETERINARIAN ABOUT MEDICATIONS THAT HELP SLOW DOWN THE PROGRESSION OF CKD
CKD has certain effects on a cat’s body. If some of them can be reduced or at least managed effectively, it improves the affected cat’s quality of life and makes things a bit easier for the owner as well.
A medication exists that reduces the amount of protein lost in the urine of a cat suffering with CKD. Speak to your veterinarian for more information.
STAY FOCUSED
REMEMBER: The purpose of all your dedicated efforts is to give your cat the best chance at a happy life which entails improving his or her life and lifespan. The two goes hand in hand. After all, helping your cat live longer without making him or her feel better wouldn’t be fair.
CONNECT WITH OTHER OWNERS OF CATS WITH CKD
There are support groups for owners of cats with CKD. You may talk to others who know what you’re going through. To find a group, perhaps start your search online.
Related Articles



HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Facts About a Dog’s Heart

Studies show that people who own pets are healthier, have fewer heart attacks and live longer. Happy, healthy dogs also live longer than unhealthy, unhappy dogs. Still, just like humans, dogs can suffer from heart problems too.
Body Facts:
Here are some canine heart facts:
Litres of blood pumped per day: +/- 4 000
Beats per minute: 70 to 120 (human: 70 to 80)
Beats per day: +/- 144 000
WHAT YOU CAN DO TO HELP YOUR DOG’S HEART
Usually a fit, healthy dog has a healthy heart and good habits; regular exercise and a balanced diet helps a lot. But: what if you’re not sure? Are there signs to look out for? If you notice any of the following, your dog may not be as healthy as you think:
- Dull coat
- Dull eyes
- Lack of energy
- Loss of appetite
- Presence of parasites
- Discharge from the eyes, ears or nose
DON’T UNDERESTIMATE DIET
When it comes to a dog’s diet, many veterinarians believe in balance, that is, everything in moderation. In terms of heart health, the keywords are lean and clean. Combine this with exercise and you already have an advantage. Go the other route and you’re bound to hurt your dog’s heart. In most cases, these guidelines will apply, so try to invest in dog food brands with high quality ingredients chosen for their nutritional value. Ask your veterinarian for recommendations as well. He or she will know which brands (and amounts) are most beneficial for your dog’s age, weight and health needs.
FACTS ABOUT A DOG’S CIRCULATORY SYSTEM
A dog’s heart sits between the lungs, behind the 3rd and 6th rib. The main function of the circulatory system (also known as the cardiovascular system) is to transport blood, nutrients, gases and hormones to and from the cells throughout the body. This system features heart and blood vessels (arteries, veins and capillaries) which carry blood to organs, tissues and cells. Waste and carbon dioxide are carried away plus body temperature is regulated, amongst other things.
EXERCISE REMAINS IMPORTANT
This topic comes up often, because it’s important and the benefits for both owners and dogs are incredible. For the best results, set aside time each day to walk, play with and train your dog. Just remember to take your dog’s health, age and size or breed into consideration. If you’re not sure what’s best for your dog, ask your veterinarian.
DON’T FORGET TO GO FOR CHECK-UPS
Puppies should visit a veterinarian as often as recommended, while adolescent and adult dogs must see a veterinarian at least once a year. Keep documenting any questions you may have before your next visit and take advantage of your annual check-up to ask away.
In between visits, be sure to use preventative products for internal and external pests and parasites.
Related Articles
A Heart-to-heart about Pet heart health Read Now
Heart Disease In Dogs Read Now
What You Need To Know About Heart Attacks In Dogs Read Now
Congestive Heart Failure (CHF) As a Result Of Dilated Cardiomyopathy (DCM) Read Now
Congestive Heart Failure (CHF) As a Result Of Atrioventricular Valvular Insufficiency (AVVI) Read Now

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
World Rabies Day – awareness and prevention efforts

Rabies spreads when the saliva of an infected animal – through a bite or otherwise – comes into contact with broken skin (which includes scabs) or the eyes, nose or mouth of another animal or person.
World Rabies Day
Rabies is a deadly virus and survival is highly unlikely. Once contracted it may affect the spinal cord and cause inflammation in the brain. However, growth starts in the muscle tissue before attacking the nervous system and spreading.World Rabies Day, created and coordinated by Global Alliance for Rabies Control (GARC), is observed annually on 28 September. World Rabies Day is a global health observance that was started in 2007. Governments, organisations and individuals hold events on this day that highlight their work and educate their communities. GARC provides an event platform and resources to increase their impact and share their work with other rabies stakeholders across the world.
WORLD RABIES DAY IS A GLOBAL DAY OF ACTION AND AWARENESS FOR RABIES PREVENTION. THE GOALS ARE TO:
- RAISE AWARENESS ABOUT PREVENTION
- ENCOURAGE PREVENTION
2024’S MESSAGE IS, “BREAKING RABIES BOUNDARIES”.
The focus on 2024’s theme highlights the critical need to overcome the obstacles impeding our battle against this deadly disease.
WE ALSO ENCOURAGE TO PROMOTE THE FOLLOWING:
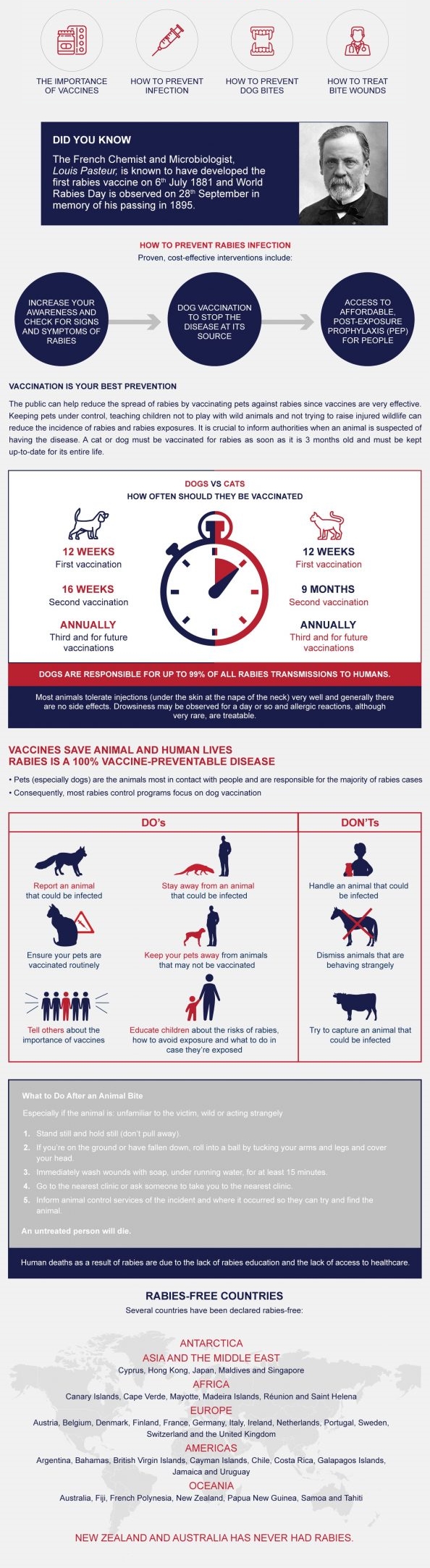
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Rabies diagnosis, prevention & the value of vaccination

Rabies is a dangerous, fatal viral disease that can be contracted by animals and humans. Animals are typically the transmitters and dogs alone are responsible for 99% of related deaths. For this reason, prevention efforts should primarily be focused on canines.
WHAT CAN INCREASE A PET’S ODDS OF BECOMING INFECTED?
- Not receiving routine vaccines
- Exploring alone / without supervision
- Coming into contact with an unvaccinated animal
HOW IS RABIES DIAGNOSED?
Brain samples taken after death are required to make a reliable diagnosis. So, even though there are several signs of rabies infection, diagnosis can only be confirmed once the affected mammal has succumbed to the disease.
Before the disease takes its toll, veterinarians can only consider clinical symptoms and the animal’s history.
If rabies has been confirmed in a dead animal that attacked another before it died, the victim will most likely have contracted rabies from it. The necessary measures, generally recommended by a veterinarian, should be taken.
HOW CAN RABIES BE PREVENTED?
BE A RESPONSIBLE PET OWNER

Note: If you think a deceased pet is carrying rabies, rather contact animal control services to help you take him or her to the veterinary. Diagnosis may provide peace of mind and inform further action if anyone else (animal or human) is at risk.
BE SAFE
If you have the smallest suspicion that your pet may have been exposed to the rabies virus, don’t ignore your instincts. Safely transport your pet to the nearest veterinary for inspection. Be careful around his or her mouth and rather wear thick gloves if you have a pair handy.
DID YOU KNOW
World Rabies Day is observed annually on 28 September to raise awareness about rabies prevention.
It is the first and only global day of action and awareness for rabies prevention. Individuals, NGOs and governments are therefore encouraged to use this opportunity to create awareness and encourage prevention.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Congestive Heart Failure (CHF) as a Result of Dilated Cardiomyopathy (DCM)

Did you know that canine heart disease is just as dangerous in dogs as it is in people?
HOW DOES THE HEART WORK?
The heart is one of the most miraculous “machines” that works like a pump and beats thousands of times per day.
- The heart is a combination of 2 pumps, and each pump has 2 chambers.
- The 2 pumps are divided by Left and Right sides.
- The blood enters the right side and is then pumped to the lungs, where the blood is oxygenated.
- The oxygen rich blood then flows into the left side of the heart, and from there it is pumped out into the body’s various organs.
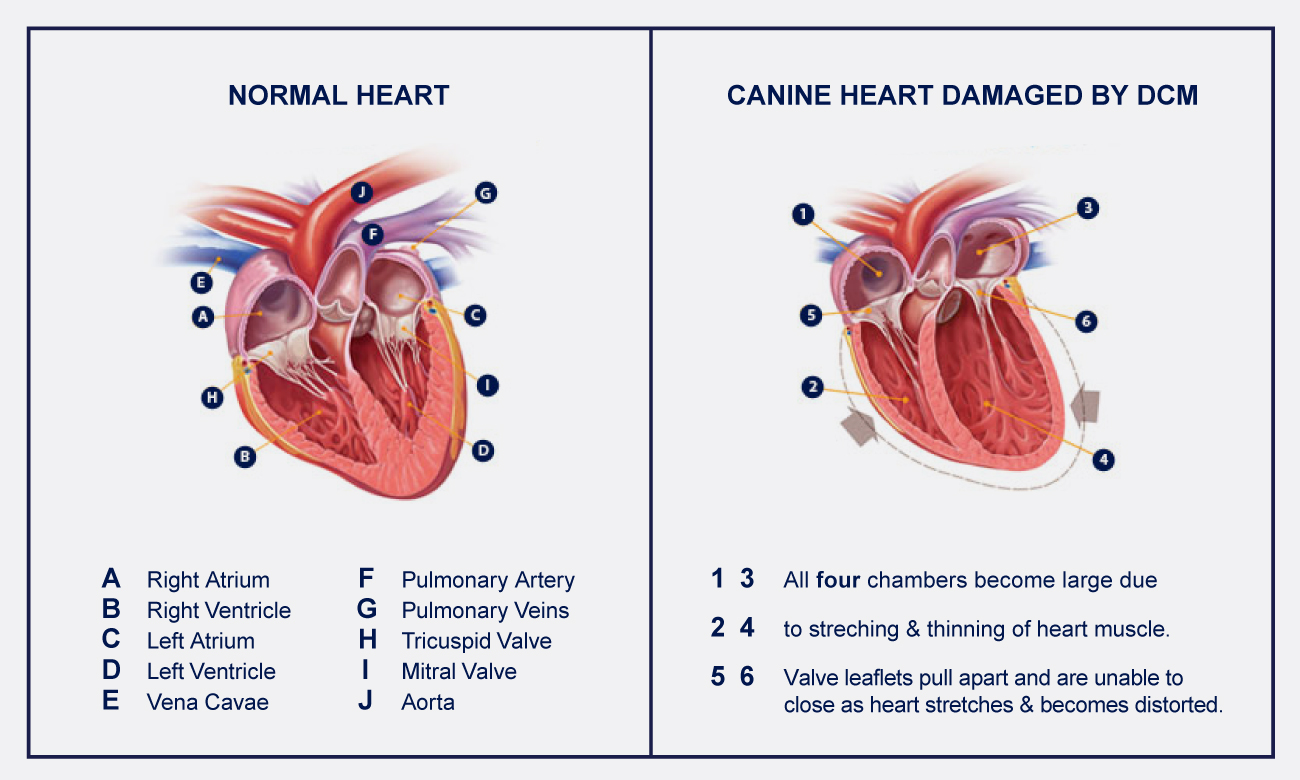
WHAT IS DCM?
DCM is the second most common form of heart disease in a dog.
DCM is a disease of the heart muscle itself where the dog’s heart fails to pump effectively. Heart contractions are weak and therefore blood is not pumped through the body efficiently.
Typically, the heart stretches and enlarges, which over time further decreases its ability to pump blood around the body.
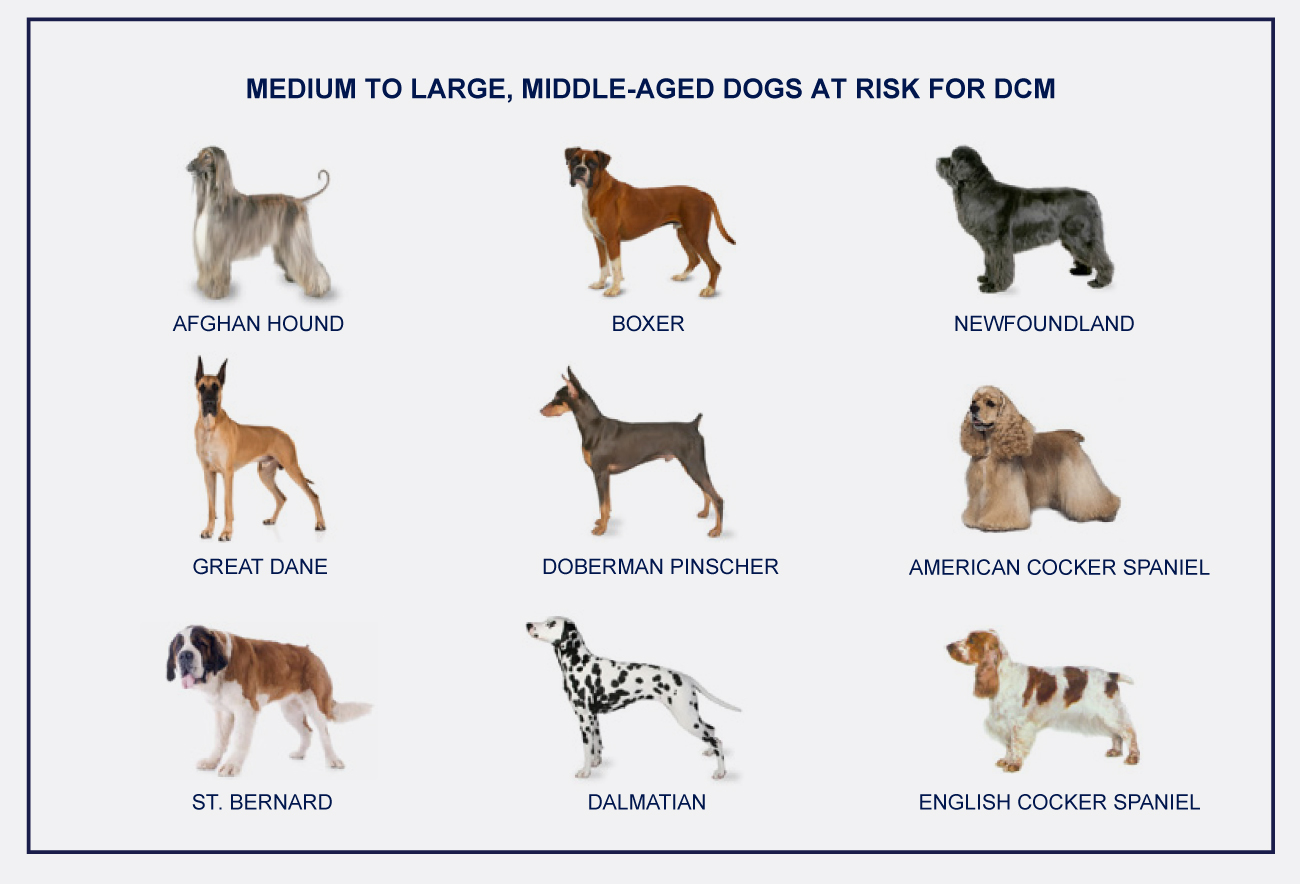
DON’T LOSE HOPE
With early diagnosis and appropriate treatment and management, you increase your dog’s opportunity to live a happier, healthier and longer life.
WHAT ARE THE CAUSES OF HEART DISEASE?
There are several ways your dog can be affected by heart disease:
Acquired Heart Disease
- Accounts for 95% of all heart conditions
- Disease that develops during the course of your dog’s life
- There are two principal causes of acquired heart disease:
– Valvular disease, which is also known as atrioventricular valvular insufficiency (AVVI)
– Dilated cardiomyopathy (DCM)
Congenital Defects
- Heart problems that your dog is born with
- Will usually be diagnosed when your dog is still a puppy
- Account for a very small percentage of the diagnosed heart-related problems
SIGNS OF DCM
In the early stages, signs of atrioventricular valvular insufficiency (AVVI) or dilated cardiomyopathy (DCM) are most likely to be subclinical. This preclinical phase can last for months or years. However, as the heart deteriorates and cardiac output decreases over time, AVVI and DCM ultimately lead to congestive heart failure (CHF) in dogs.
Common clinical signs of CHF that may appear as AVVI or DCM progresses include:
- Breathing changes
- Increased heart rate
- Difficulty breathing
- Shortness of breath
- Coughing
- Behavioural changes
- Lack of energy
- Depressed or withdrawn
- Exercise intolerance
- Easily tires
- Hesitates to go for walks
- Poor appetite and weight loss
- Weakness and fainting
- Restlessness, especially at night
As soon as clinical signs of DCM appear, it’s important to get therapeutic intervention immediately.
No cure for DCM exists and surgical intervention is rarely practical in canine patients, so therapeutic goals focus on improving clinical signs and prolonging life.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Congestive Heart Failure (CHF) as a Result of Atrioventricular Valvular Insufficiency (AVVI)

Did you know that canine heart disease is just as dangerous in dogs as it is in people?
HOW DOES THE HEART WORK?
The heart is one of the most miraculous “machines” that works like a pump and beats thousands of times per day.
- The heart is a combination of 2 pumps, and each pump has 2 chambers.
- The 2 pumps are divided by Left and Right sides.
- The blood enters the right side and is then pumped to the lungs, where the blood is oxygenated.
- The oxygen rich blood then flows into the left side of the heart, and from there it is pumped out into the body’s various organs.
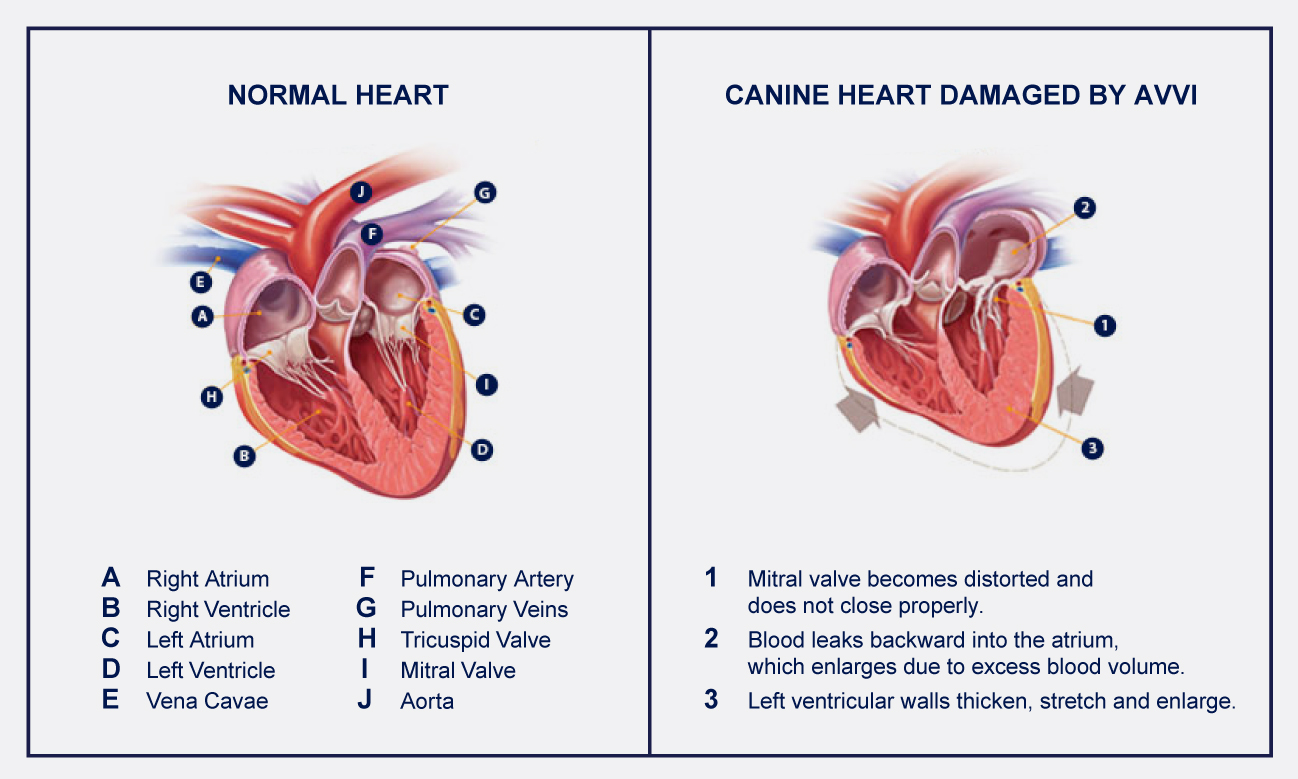
WHAT IS AVVI?
AVVI is the most common cause of CHF in dogs.
AVVI is a degenerative disease that damages heart valve leaflets. This damage prevents heart valves from closing properly, allowing blood to leak backward into the atrium. This leakage eventually impairs heart function and circulation, leading to CHF.
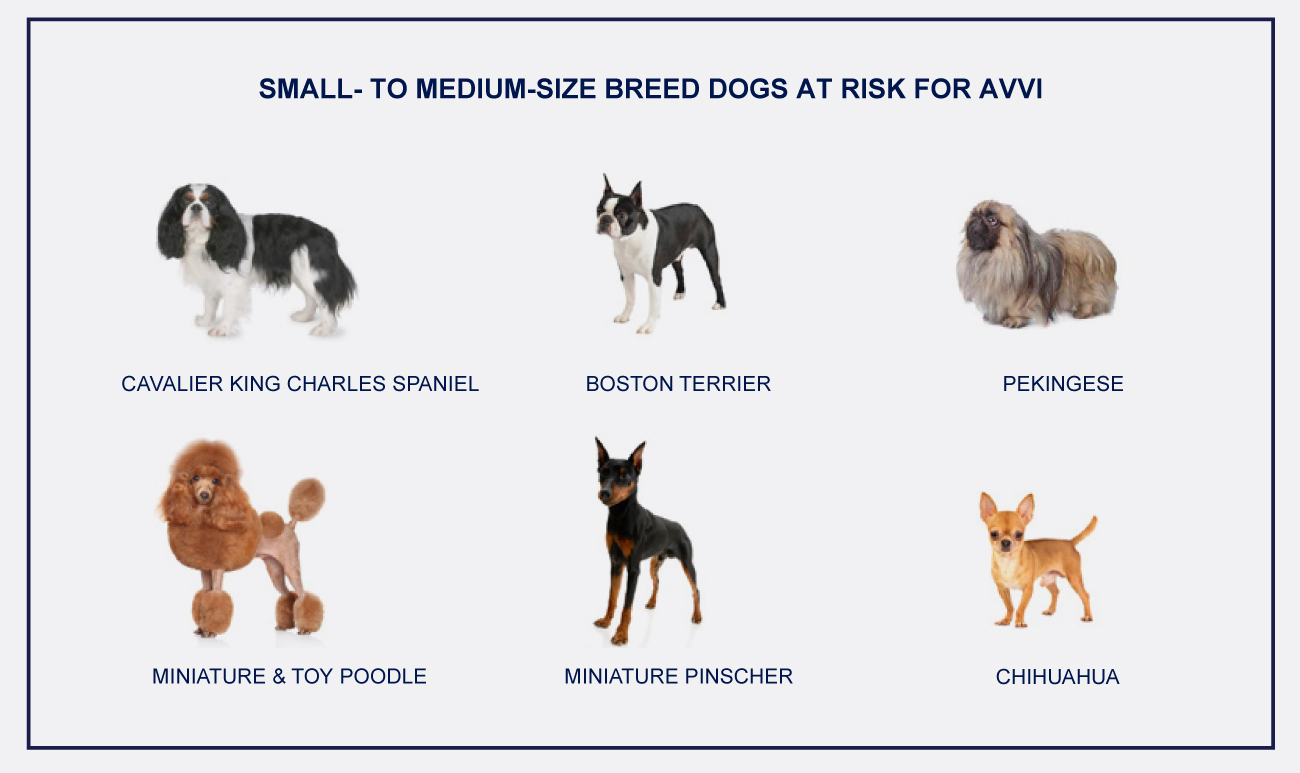
DON’T LOSE HOPE
With early diagnosis and appropriate treatment and management, you increase your dog’s opportunity to live a happier, healthier and longer life.
WHAT ARE THE CAUSES OF HEART DISEASE?
Your dog can be affected by heart disease in several ways:
Acquired Heart Disease
- Disease that develops during the course of your dog’s life
- Accounts for 95% of all heart conditions
- The two principal causes of acquired heart disease:
– Valvular disease, known as atrioventricular valvular insufficiency (AVVI)
– Dilated cardiomyopathy (DCM)
Congenital Defects
- Heart problems that your dog is born with are usually diagnosed when your dog is a puppy
- Account for a very small percentage of the diagnosed heart-related problems
SIGNS OF CHF
Symptoms of atrioventricular valvular insufficiency (AVVI) or dilated cardiomyopathy (DCM) in the early stages are not readily observable. This phase can last for months or years. However, as the heart deteriorates and cardiac output decreases over time, AVVI and DCM ultimately lead to congestive heart failure (CHF) in dogs.
Some common clinical signs of CHF that may appear as AVVI or DCM progresses include:
- Breathing
- Difficulty breathing
- Increased heart rate
- Shortness of breath
- Coughing
- Behavioural changes
- Tires easily
- Withdrawn
- Exercise intolerance
- Hesitates to go for walks
- Decreased appetite and weight loss
- Weakness and syncope (fainting)
- Difficulty sleeping
- Restlessness, especially at night
When clinical signs of CHF appear, immediate therapeutic intervention is indicated.
There is no cure for CHF and surgical intervention is rarely practical in dogs, so veterinarians focus on improving clinical symptoms and prolonging life.
Related Articles








TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Health Issues & Conditions in Specific Dog Breeds

A big part of a dog’s general wellbeing is their health. Unfortunately some breeds are more likely to suffer from certain conditions than others.
These breeds are:
- Bulldogs
- Beagles
- Boxers
However, they’re not the only ones. Before choosing to adopt or buy one of these breeds you should know about the potential health problems they can be born with. Health problems can start affecting dogs while they’re puppies, adolescent dogs or adult dogs.
If you own one of these breeds (including the ones we’ll discuss below) it’s important to be aware of health issues that could affect your dog. Any changes in behaviour or physical appearance should be discussed with your veterinarian.
Tests can rule out or confirm issues and if necessary your veterinarian should recommend a plan to manage the symptoms and reduce complications.
BLOAT
Dogs likely to suffer from bloat: Great Danes, Saint Bernards and other giant and large breeds.
What happens: Internal organs can suffocate when the stomach twists and traps gas inside. This reaction is caused by the shape of their chests which can make their stomachs swell with liquid and gasses.
How to help prevent and deal with bloat: If you have a giant or large breed, place food in a raised bowl or make use of an elevated feeder. Also regularly check your dog’s stomach. If it seems tight or swollen a careful examination can be performed by your veterinarian.
HIP OR ELBOW DYSPLASIA
Dogs likely to suffer from hip or elbow dysplasia: Golden and Labrador Retrievers, German Shepherds and other large breeds.
What happens: Hip dysplasia can cause lameness, arthritis and loss of mobility due to the abnormal formation of the hip socket that causes serious pain. Elbow dysplasia, which can cause lameness, occurs in the joints of the front legs.
How to help prevent and manage hip dysplasia: Avoid overfeeding and make sure your dog exercises regularly.
How to help prevent and manage elbow dysplasia: Elbow dysplasia can be treated. Options include medication and surgery.
ARTHRITIS AND JOINT PAIN
Arthritis and joint problems are not breed-specific conditions. Dogs usually experience arthritis and joint problems when they grow older, but it’s usually treatable. Joint problems, manifesting as lameness, can also occur earlier, mostly in larger breeds.
How to help dogs with arthritis and joint pain: Weight management, exercise and pain medication can all help reduce pain and manage the condition. Some dogs may even grow out of it.
EYE DISEASES
Dogs likely to suffer from glaucoma and cataracts early in life: Beagles, Chow Chows and Poodles. Dogs likely to suffer from glaucoma and cataracts later in life: Most breeds (it’s part of ageing).
Progressive Retinal Atrophy (PRA) AKA Progressive Rod-cone Degeneration (PRCD): This group of eye diseases, which can eventually lead to blindness in both eyes, can start affecting dogs at an early age.
HEART DISEASES
Heart diseases and related conditions in general are not limited to certain breeds and dog sizes. Regular medication is often required and exercise should be kept to a minimum in some cases.
Congestive heart failure (CHF) can be caused by atrioventricular valvular insufficiency (AVVI), dilated cardiomyopathy (DCM) and mitral valve disease (MVD).
- AVVI: Most common in small to medium sized breeds such as Cavalier King Charles Spaniels, Miniature and Toy Poodles, Schnauzers, Chihuahuas and Yorkshire Terriers.
- DCM: Most common in Doberman Pinschers, Great Danes, Boxers and Cocker Spaniels.
- Mitral valve disease: More common in smaller breeds e.g. Poodles, Yorkies, Pugs and Pomeranians.
Congestive heart failure (CHF) can also be caused by inherited defects such as aortic stenosis, subaortic stenosis (SAS), tetralogy of fallot (TOF), ventricular septal defects (VSD) and persistent ductus arteriosus (PDA).
- Aortic stenosis and SAS: Breeds susceptible to subaortic stenosis include Newfoundlands, German Shepherds, Golden Retrievers, Rottweilers and Boxers (larger breeds).
- TOF: More likely to occur in purebred dogs, specifically English Bulldogs and Keeshonds.
- VSD: Appears sporadically in many different dog breeds.
- PDA: The most commonly affected breeds are Maltese, Poodle, Pomeranian, Keeshond, Bichon Frise, Chihuahua and German Shepherd.
Other heart conditions include:
- Tricuspid valve dysplasia: Susceptible breeds include Labrador Retrievers and German Shepherds.
- Hypertrophic cardiomyopathy: Uncommon, but most frequently seen in young to middle-aged large breeds such as Rottweilers, Dalmatians, German Shepherds, Boston Terriers and certain Pointers (males are more susceptible).
Before choosing a breed, learn more about their potential health issues. If possible, get both parents’ medical histories. Also make sure the breed you choose fits in with your lifestyle.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Eye Inflammation (Anterior Uveitis) in Cats

WHAT IS ANTERIOR UVEITIS IN CATS?
Uveitis is one of the most common eye disorders in cats and can be extremely serious. Without medical attention, your cat’s eyesight is at great risk.
Uveitis is inflammation of the uvea, which is the dark tissue at the front of the eye that contains the blood vessels. This includes the iris (the coloured layer around the pupil), ciliary body, and choroid (see diagram below).
When the uvea becomes inflamed, the condition is referred to as anterior uveitis (inflammation of the front of the eye).
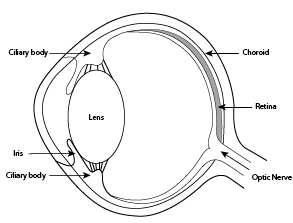
WHAT ARE THE SYMPTOMS OF ANTERIOR UVEITIS?
Uveitis can have many clinical signs. The most common symptom of uveitis is a colour change to the eye(s) that may be cloudy or red.
Other symptoms may include:
- Pain
- Squinting
- Pawing at the eye
- Sensitivity to light
- Redness in the white part of the eye
- Excessive tearing
- Watery discharge
- Abnormal size or uneven shape of pupil
- Swollen eyeball
- Cloudiness or dullness of the front of the eye
- The colour of the iris may be different than normal or uneven
- Redness or protrusion of the third eyelid
WHAT ARE THE CAUSE OF ANTERIOR UVEITIS?
The cause can often be challenging to identify, even with extensive diagnostic tests.
Common causes of anterior uveitis in cats include:
- Tumours
- Cancers
- Autoimmune diseases
- Metabolic diseases
- Lens protein entering into the eye fluid
- Trauma or injury
- Viruses
- Infections: Fungi; Bacteria; Parasites; Rickettsia (a parasitic disease found in many ticks, fleas and lice)
WHAT IS THE TREATMENT FOR ANTERIOR UVEITIS?
Treatment will depend on the underlying cause. It generally consists of prescribed drops or ointments to put in the cat’s eye, as well as oral medications to reduce any pain or inflammation.
If an infection is found, an antibiotic topical drug will be prescribed. If the underlying cause is a fungus, anti-fungal drugs will be prescribed.
In some situations for example, if there is a tumour, the veterinarian may recommend surgery to remove the eye.
Luckily, there is treatment that brings pain relief.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What You Need to Know About Epilepsy in Dogs

Epilepsy is a brain disorder that is more common in dogs than in cats. It’s also important to know that a seizure is a single occurrence while the word epilepsy is used when two or more unprovoked seizures have occurred.
This article will look at causes, symptoms, what to do when your dog has a seizure and different types of epilepsy.
What Happens When a Dog Experiences a Seizure?
Before a seizure a dog can seem confused or dazed. During a seizure you may notice the following changes in appearance and behaviour:
- Stiffening
- Collapsing
- Urination and defecation
- Conscious or unconscious
- Jerking and muscle twitching
- Flailing limbs (as if treading water)
- Drooling and foaming at the mouth
- Twitching or uncontrollable shaking
- Falling to the floor, usually on their side
- Jaw motion and possible chewing of the tongue
An episode can last from about 30 seconds to a few minutes. Once the episode is over you may notice disorientation, unsteadiness, bumping into objects, walking in circles and even temporary blindness. The area around the mouth may still have some drool or foam and there could be blood if there was chewing or biting. It’s also not uncommon if a dog seeks a spot to hide for a while.
What Causes Epilepsy in Dogs?
Certain conditions and medical problems can lead to abnormal, uncontrolled bursts of electrical activity in a dog’s brain.
- Strokes
- Anaemia
- Head injury
- Brain cancer
- Liver disease
- Kidney disease
- Ingesting poison
- Electrolyte problems
- Low or high blood sugar
- Encephalitis (inflammation of the brain, caused by infection or an allergic reaction)
Types of Seizures in Dogs
- Idiopathic: The cause of this type of epilepsy is unclear.
- Grand mal (generalised): The most common type of seizure. It affects the whole brain. A dog will lose consciousness and convulse for anything from a few seconds to a couple of minutes.
- Focal: Only a part of the brain experiences abnormal electrical activity that leads to a seizure. It affects one limb or one side of the body, causing it to move in an unusual way.
- Psychomotor (complex partial): during this type of seizure a dog does not seem to be aware of its surroundings and will repeat a specific bizarre activity for a couple of minutes, whether it’s chasing its tail or some imaginary object.
The following dogs are more prone to suffer from idiopathic epilepsy: Australian Shepherd, Beagle, Belgian Tervuren, Border Collie, Collie, German Shepherd and Labrador Retriever.
A focal seizure can turn into a grand mal seizure.
What You Can Do if Your Dog has a Seizure?
- It won’t be easy, but stay calm for your dog’s sake
- You can speak to your dog in a soft, soothing voice
- Don’t touch or go near your dog’s head, especially the mouth to avoid biting
- Like humans, dogs won’t choke on their tongues, so don’t put anything in his mouth
- Remove dangerous objects and block dangerous areas or slide him away from them
- If a seizure continues for more than three minutes, you need to prevent overheating: cool the paws with water, blast the air conditioning or turn on a fan
Once the episode comes to an end you should probably contact your veterinarian.
You should head to the nearest veterinary if your dog has a long episode (near or more than five minutes) or more than one seizure in a row, as either might cause breathing issues and possible brain damage. The veterinarian will take it from there.
What will Happen at the Veterinarian’s Office?
- Blood tests
- Physical exam
Your veterinarian could prescribe anticonvulsants. It’s extremely important to follow the instructions with regards to both dosage and frequency of medicating.
Related Articles
HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Epilepsy & Seizures in Dogs

SEIZURES DON’T JUST HAPPEN TO HUMANS
Pets, including dogs, can also suffer from seizures. They occur when there is ‘explosive’ electrical activity in the brain and are often described as an uncoordinated firing of the neurons.
Why neurons do not function normally is not understood, but probably certain substances called neurotransmitters are not in the proper chemical balance, so the nerves do not behave in the normal coordinated fashion.
Epilepsy is a disorder of recurring bouts of uncoordinated firing of the neurons within the brain. These episodes are called seizures and occasionally are referred to as convulsions or “fits.”
TYPES OF EPILEPSY IN DOGS
Epilepsy can be broadly categorised into two types: primary (or idiopathic) and secondary (or symptomatic).
Primary epilepsy: also known as idiopathic (unknown cause), genetic, inherited, or true epilepsy. Most dogs that are diagnosed with epilepsy have primary epilepsy, where no underlying cause for the seizures is found. These dogs will be healthy and completely normal in all other respects.
Breeds most prone to idiopathic epilepsy include the:
- Beagle
- Boxer
- Keeshond
- Belgian Tervuren
- Golden & Labrador Retriever
- Dachshunds
- Vizsla
- Shetland Sheepdog
- German Shepherds
- Poodle
- English Springer Spaniel
- Irish Setter
Secondary epilepsy refers to seizures for which a cause can be determined, and there are many.
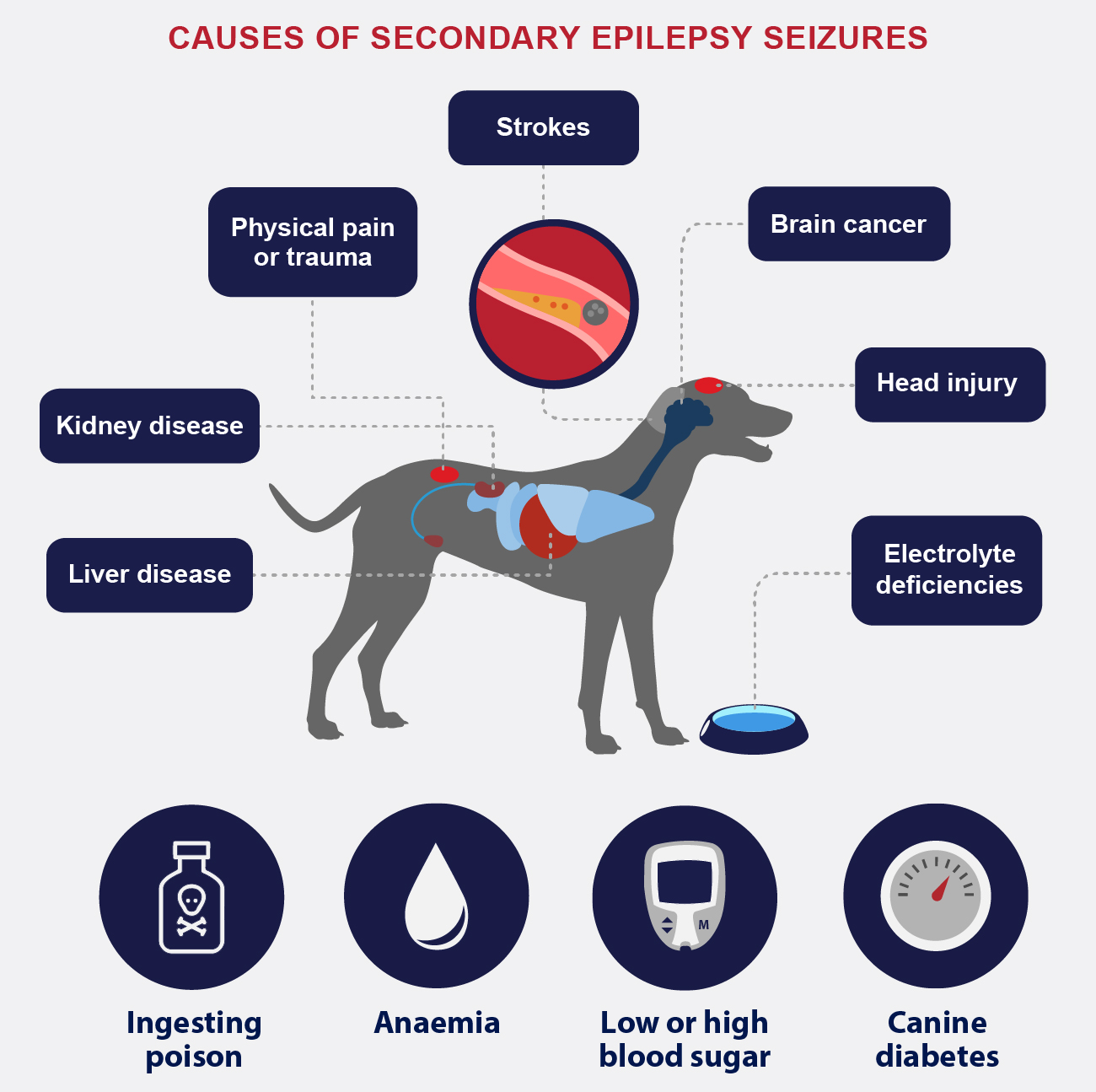
TYPES OF EPILEPSY SEIZURES IN DOGS
Based on the type of behaviour and brain activity, seizures are divided into two broad categories:
- generalised
- focal (also called partial or local)
Some dogs have more than one type of seizure, and not all seizures involve convulsions. Most epileptic fits usually happen quite suddenly without warning, last a short time (often only a few seconds or minutes) and stop by themselves.
The following types of seizures describe what happens during the attack.
1. GENERALISED SEIZURES
Generalised seizures may occur alone or may start as a focal seizure and become a generalised seizure (see point 3 below). In most cases of generalised seizures the dog loses consciousness, and salivation, urination and defecation may occur. Motor movement occurs on both sides of the body. Aspects of generalised seizures are often termed tonic-clonic , tonic, clonic, myoclonic and atonic. These terms are defined below:
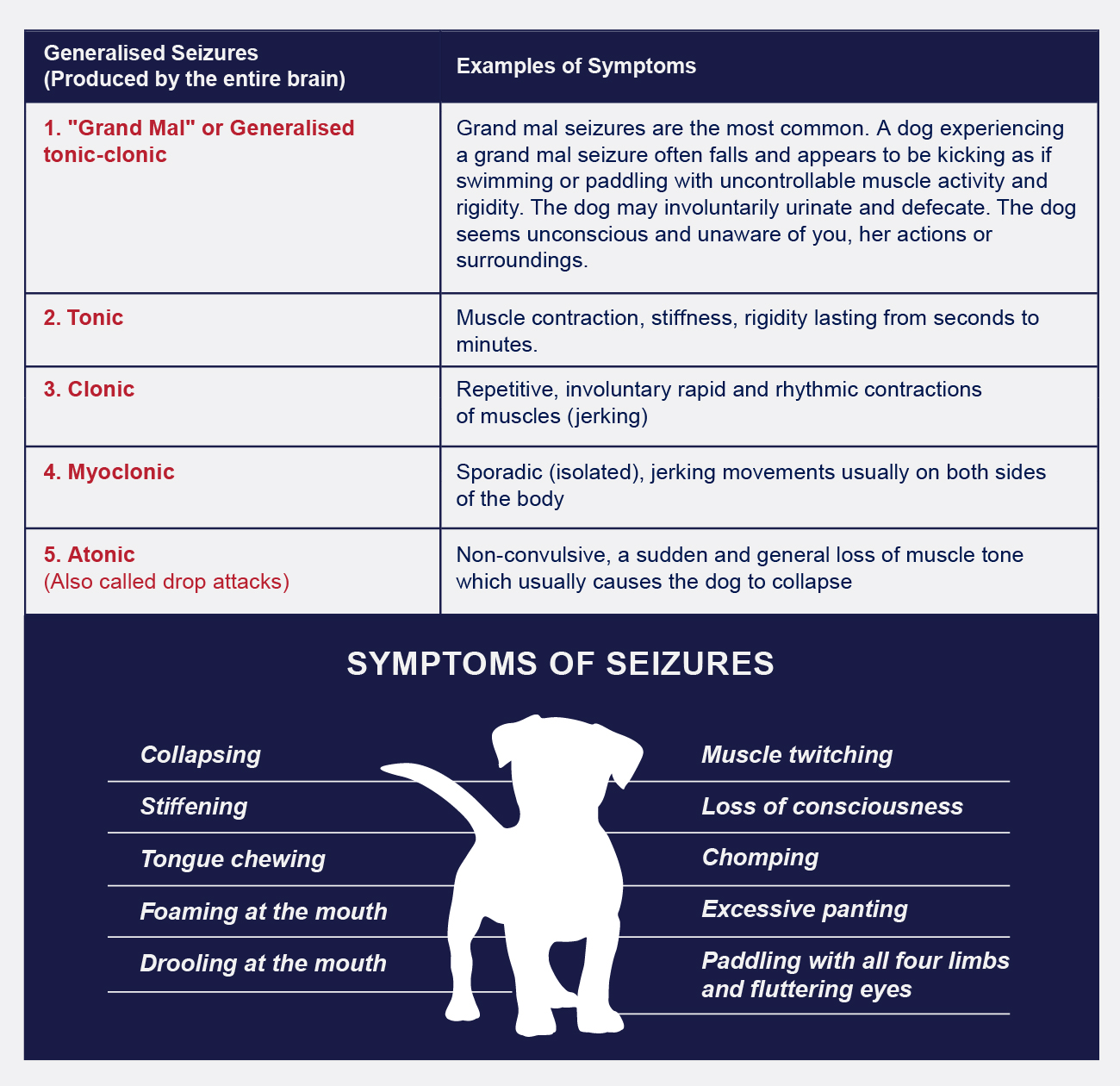
2. FOCAL (PARTIAL OR LOCAL) SEIZURES
These only occur in one half of the brain and within a particular region. How these types of seizures present themselves depends upon where in the brain the abnormal electrical activity started, and the function of that part of the brain. Focal epileptic seizures can have these symptoms:
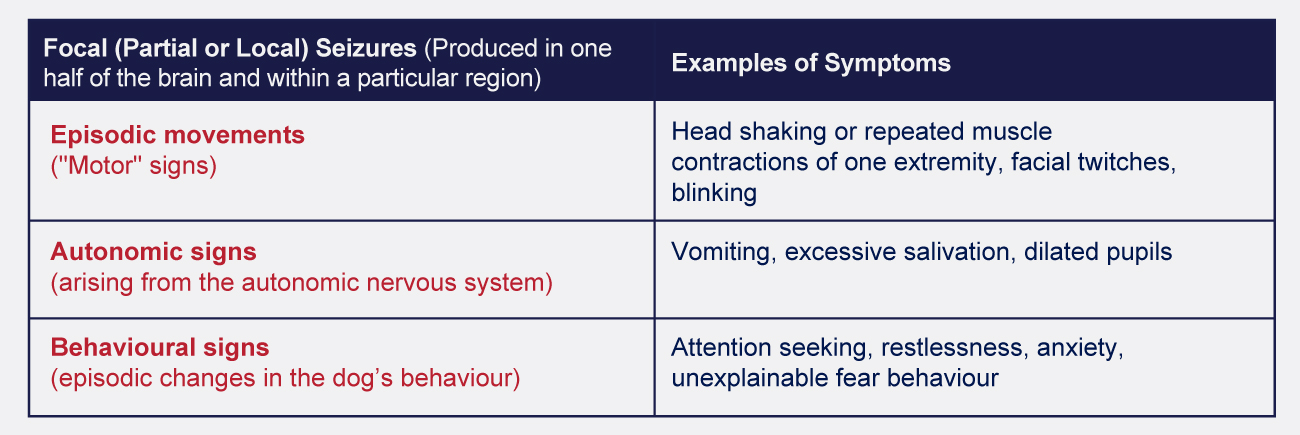
3. FOCAL (PARTIAL OR LOCAL) SEIZURE CHANGING INTO A GENERALISED SEIZURE
A focal (partial or local) seizure can change into a generalised seizure. This is the most common seizure type observed in dogs. The focal seizure is often very short (a few seconds to minutes) and the generalised seizure follows rapidly. The focal seizure may be difficult to detect due to its brief nature and it is important to tell your veterinarian what happened before convulsions started, to help them determine what type of seizure your dog is having.
Related Articles
HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
What To Do During A Dog’s Seizure

WARNING SIGNS OF EPILEPTIC SEIZURES IN DOGS
There are often warning signs when a dog is about to have a seizure. A dog may begin to act scared, dazed, stressed or anxious without cause. Dogs may also have trouble seeing, experience muscle and limb contractions, and even lose bowel and bladder control. Before a seizure, dogs may look dazed, seem unsteady or confused, or stare off into space. Dogs seem to have a “sixth sense” about certain upcoming events. Dogs have been known to seek companionship immediately before seizures while others may try to hide.

SYMPTOMS OF EPILEPTIC SEIZURES IN DOGS
Once the seizure(s) begins, the dog may fall on one side and become stiff. The dog may chomp its jaw, salivate profusely, pant excessively, drool or foam at the mouth, urinate, defecate, vocalise, and/or paddle with all four limbs. There may be jerking, muscle twitching, tongue chewing or even loss of consciousness. Seizure activities generally last between 30 and 90 seconds. If a seizure lasts over five minutes, your dog is more at risk of falling into a coma or having internal organ damage. In the instance of a partial seizure, the seizure will only affect a small part of the dog’s brain, and be seen in only one limb, one side of the body, or just its face.

WHAT TO DO DURING A DOG’S SEIZURE
It is important to remain calm and provide reassurance to the dog that all will be fine. Panicking will only increase the dog’s anxiety. Remove any items that could hurt the dog during the seizure. Remove children and other pets from the area.
Stay away from the dog’s mouth, as you could get unintentionally bitten. A dog can’t choke on its tongue, so there’s no need to worry about that.
If the seizure continues for more than a couple of minutes, the dog will be at risk of overheating. Turn a fan on and pour cold water on the dog’s paws to help him cool down.
Observe your dog closely. As soon as the seizure ends, make sure to call your veterinarian.
If the dog has a seizure that lasts more than 5 minutes or if he has several in a row while he’s unconscious, take him to a veterinary as soon as possible. The longer a seizure goes on, the higher a dog’s body temperature can rise, and he may have problems breathing. This can raise his risk of brain damage.

POST-SEIZURE SYMPTOMS
Some dogs may act as if nothing happened after the seizure(s) while others will show altered behavioural characteristics. This includes periods of confusion and disorientation, aimless wandering, compulsive behaviour, momentary blindness, pacing, increased thirst, and even an increased appetite. Recovery may be immediate or take up to 24 hours. Younger dogs seem to have more severe epilepsy. When the onset is before the age of two, the condition will respond positively to medication. But the more seizures a dog has, the more likely there is to be damage among the neurons in the brain.
Seizures are best met head on, so early detection and treatment is essential.
Related Articles
HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Dog Epilepsy Can Be Managed

IS YOUR DOG EXPERIENCING EPILEPTIC SEIZURES?
Epilepsy in dogs is a common condition that cannot be cured, but it can be managed so your dog can have a full and happy life. Successful management requires lifelong medical attention and knowing what to do to best manage your dog’s condition.
WHAT TO DO DURING A SEIZURE
Watching your dog have a seizure is terrifying.
It’s important to remember that:
- When a dog has a seizure, as difficult as it may be, it is important to remain calm.
- Seizures themselves are almost never fatal.
- Dogs do not swallow their tongues during seizures.
- You should never put your hands or anything near or in a seizuring dog’s mouth.
DOG SEIZURE FIRST AID
- Don’t panic.
- Keep people or pets away.
- Gently try to calm and soothe your dog.
- Make the dog as comfortable as possible – do not hold the dog down.
- If necessary gently move your dog to a safe place or lay your dog down on a rug to minimise the chances of injury.
- Prevent injury – make sure nothing is in reach that could harm the dog if struck.
- Some dogs are light or sound sensitive during seizure episodes. Try dimming the lights and keeping phones at a distance from the dog.
- If the seizure lasts for more than a few minutes, turn a fan on and pour water over his paws as he may overheat.
- Keep old towels handy to catch urine if your dog urinates during seizures.
- Do not give the dog water or food until fully alert.
- Many dogs are confused and even blind right after a seizure. Keep the dog in a safe area where they cannot fall down stairs or hurt themselves.
WHAT TO DO DURING A DOG’S SEIZURE
- REMAIN CALM
- REMOVE any items, that could hurt your dog, out of the way
- STAY AWAY FROM YOUR DOG’S MOUTH – Your dog cannot choke on his tongue so you don’t need to worry about this.
- If the seizures last more that a few minutes turn a fan on him/her and pour cold water on his/her paws as your dog may overheat.
- When the seizure ends, CONTACT YOUR VETERINARIAN IMMEDIATELY.
DOG SEIZURE LOG
It’s important to give your veterinarian a clear and accurate account of your dog’s behaviour before, during and after the seizure. This valuable information will help your veterinarian identify any patterns and make decisions on the most appropriate management and treatment options.
- Keep a careful diary of the seizures. Make a video recording if possible.
- As soon as possible write down the exact time the dog started to seizure and the time the seizure ended.
- Note what your dog was doing before the seizure and whether there was any unusual behaviour.
- Note any unusual behaviour after the seizure.
- Comment on any changes that may have contributed to the seizure such as, changes in environment, food or medications.
The diary will indicate if a seizure followed an event more than one time.
HOW LONG DO SEIZURES LAST?
Generally a seizure will only last for a couple of minutes.
Contact your veterinarian immediately if:- your dog’s seizure lasts more than five minutes
- your dog has more than one seizure in a 24 hour period
- your dog is a young puppy or a lactating bitch
HOW IS EPILEPSY TREATED?
Anticonvulsant drugs are commonly needed to control seizures. It is important to know that seizures are rarely eliminated completely. The goal of therapy is to reduce the frequency and severity of seizures so that the dog can live a comfortable, happy and full life.
Related Articles
HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
OSTEOARTHRITIS IN CATS

Cats are natural survivors and masters at hiding pain, which means discomfort and illness often go unnoticed.
If owners and veterinarians can’t see any issues, no diagnosis can be made which means symptoms and pain caused by diseases go untreated.
Osteoarthritis (OA), also known as degenerative joint disease (DJD) is one of the diseases that are easy to miss.
Once correctly diagnosed, medication can relieve joint pain caused by osteoarthritis.
HOW COMMON IS OA?
According to numerous studies, many of which analyse radiographs, an alarming number of (especially older) cats suffer from degenerative joint disease in one form or the other. The studies have helped us realise that DJD is very common in cats and even more severe in older cats. Most affected joints include lumbar spine, shoulders, hips, elbows, knees and ankles.
OA CAUSES
Joints are cushioned by cartilage, a rubbery connective tissue, found at the ends of bones. When this cartilage starts to deteriorate it leads to inflammation and discomfort and the damage continues.
Natural wear and tear, joint injury as well as certain abnormalities may contribute to OA, but the specific causes are still unclear.
THE FOLLOWING MAY INCREASE RISK OF OA
- Obesity
- Trauma / injury, e.g. fractures or dislocations
- Certain breeds are more prone to
– Kneecap dislocation formally known as Patella luxation (e.g. Abyssinian and Devon Rex breeds)
– Abnormal hip joint development, formally known as hip dysplasia (e.g. Maine Coon, Persian and Siamese breeds)
– Abnormality of cartilage causing severe arthritis which affects multiple joints (the Scottish Fold breed particularly) - Acromegaly (unusual and uncommon): increased growth hormone secretion, caused by a tumour, leads to diabetes and/or arthritis
SIGNS OF OA
- Less mobile: jumping behaviour changes; stiffness in legs; struggles to use stairs, litter tray and cat flap, hesitates before jumping onto counters/out of windows.
- Less activity: increased sleeptime; decreased exploring and interaction; choosing more accessible sleeping spots.
- Grooming changes: less frequent; more time spent on affected joints; overgrown claws; a scruffy/matted coat.
- Change in character/mood: more solitary; irritable when handled, stroked or interacting with other animals.
- Inappropriate elimination: urinating and/or defecating in areas where they didn’t previously.
DIAGNOSING OA
- Mature cats (aged 7+) should be checked frequently and thoroughly and owners should communicate any changes and signs noticed to their veterinarian.
- A veterinarian should be able to detect issues during an examination. X-rays are recommended to make specific diagnoses and rule out other conditions.
- Blood and urine tests could help reveal other problems and help to ensure that the cat’s organs are able to cope with chronic medication.
MANAGING OA
Change your cat’s environment to improve quality of life.
- Place comfy, warm beds in easily accessible areas where your cat will feel safe
- Provide basic steps or ramps to reach higher areas
- Make sure water and food are easy to access
- Groom your cat and cut overgrown claws
- Provide a litter tray with a low side
- Ensure the cat flap is easy to use
DIET
- Manage your cat’s weight or seek help if your cat is overweight
- Ask your veterinarian about supplements such as fatty acids and decent glucosamine and chondroitin supplements to improve cartilage quality
MEDICAL TREATMENT
Non-steroidal anti-inflammatory drugs (NSAIDs) have been found very effective in treating pain and inflammation caused by osteoarthritis in cats. Your veterinarian will be able to administer the medication after telling you more about how it works and possible side effects it may have (some NSAIDs have minimal, if any, side effects). Sometimes NSAIDs can’t be administered in which case cat-friendly painkillers may be prescribed.
Ask your veterinarian which side effects to look out for and contact the clinic if you have any questions or concerns about NSAIDs.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
UPPER RESPIRATORY INFECTIONS (URIs) IN CATS

A BRIEF LOOK AT THE RESPIRATORY SYSTEM IN CATS
A cat’s respiratory system consists of the large and small airways and the lungs.
As a cat breathes air in through its nose or mouth, the air travels down the trachea, which divides into the tubes known as the right and left bronchi, then into the smaller airways called bronchioles in the lungs.
The small sacs at the end of the bronchioles are called alveoli, where there is a thin membrane between the air and the blood.
The respiratory system is designed to deliver oxygen into the blood, which distributes it throughout the body, and to remove carbon dioxide from the blood. The exchange of oxygen and carbon dioxide occurs in the alveoli.
If there is disease, this exchange fails or becomes inefficient. At this point the cat can become seriously ill.
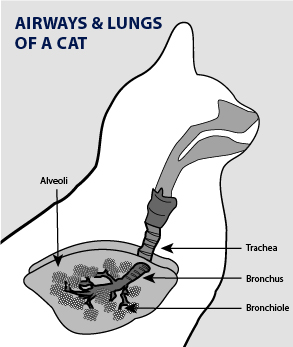
CAUSES OF UPPER RESPIRATORY INFECTIONS (URIs) IN CATS
Respiratory diseases are common in cats. Viruses are the most common cause of URIs in cats.
These viruses can be transmitted from cat-to-cat through coughing, sneezing, grooming or sharing food and water.
Cats can become carriers for life, once infected, and though they may not show clinical signs, they can still transmit the viruses to others. Cats often develop bacterial infections secondary to these common viral infections.
There are also URIs in cats that are primarily caused by bacteria, such as Chlamydia.
Cats that are kept in crowded quarters with other animals, as in a kennel, are at an increased risk of infection.
GENERAL SYMPTOMS OF URIs
Depending on the cause and location of the infection, symptoms may differ but some common clinical signs of URIs in cats include:
- Sneezing
- Difficulty breathing
- Congestion
- Runny nose
- Watery eyes
- Coughing
- Clear to coloured nasal discharge
- Gagging, drooling
- Decreased appetite
- Nasal and oral ulcers
- Squinting or rubbing eyes
- Depression
- Fever
- Pneumonia, if untreated
Related Article
Aspiration (Or Inhalation) Pneumonia In Dogs Read Now







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Epilepsy in Dogs

Not everyone knows that dogs can suffer from epilepsy. Find out everything you need to know about epilepsy in dogs.
WHAT IS EPILEPSY?
A seizure is the result of ‘explosive’ electrical activity in the brain. Epilepsy is the term used for repeated seizures.
WHAT HAPPENS DURING AN EPILEPTIC SEIZURE?
There are different types of seizures and, just like humans, not all dogs react the same when experiencing one. A seizure can be mild, for example manifesting as a lip twitching; or it can be more serious: falling to the floor and jerking around uncontrollably. It’s difficult to watch, but dogs are usually not in pain during a seizure and unaware of what’s happening (even if their eyes are open). They won’t feel great after a seizure, so continue reading to find out how you can help them.
UNDERSTANDING YOUR DOG’S EPILEPSY
There are two types of epilepsy:
- Primary (idiopathic): more common; no underlying causes; dogs are generally healthy otherwise
- Secondary (symptomatic): usually caused by a structural lesion of the brain, for example a brain tumor or vascular accident
Usually primary epilepsy is more common in the following purebred dogs, aged one to five years:
Vizslas | Boxers | Beagles | Poodles | Irish Setters | Dachshunds | German Shepherds | English Springer Spaniels | Labradors & Golden Retrievers
There’s no specific test to diagnose primary epilepsy, however, your veterinarian can examine your dog, perform blood tests (to rule out secondary epilepsy) and interpret your description of what happens during your dog’s seizure. Some veterinarians may even suggest an MRI.
MAKING SENSE OF SEIZURES
A seizure often has three phases, but remember that not all dogs are the same.
Look out for some or all of these changes:
Before a Seizure: Phase 1
- Unsettled: pacing, licking of the lips
- Heightened anxiety: whining, barking or hiding
- Excessive bodily functions: salivating or urinating
During a Seizure: Phase 2
- Making sounds
- Passing urine or faeces
- Faster, heavier breathing
- Stretched out, rigid legs; jerking or paddling movements
- Stiffening of muscles; falling to the floor on one side (with head back)
After a Seizure: Phase 3
- Your dog may not move immediately after a seizure
- The next couple of minutes to days you may see disorientation and staggered walking; temporary loss of sight; excessive hunger and thirst; uncontrolled bowel and/or bladder activity
HOW CAN YOU HELP YOUR DOG?
Firstly, whether you start noticing the signs, or realise your dog is already having a seizure, stay calm. Next do the following:
- Try to prevent injury (move objects out of the way) and don’t:- try to hold his/her head
– remove his/her tongue - If possible, remove/block/switch off things that are stimulating to the senses (TV, artificial and natural light, music playing devices, other pets, children)
- Time the length of the seizure: if it’s 5 minutes or longer or happens more than once in 24 hours, contact your veterinarian immediately
- To help your veterinarian identify patterns and recommend treatment, keep a seizure diary
- During recovery, don’t move your dog, just keep an eye on him/her
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Anaemia Due to Iron Deficiency in Dogs

OVERVIEW
Anaemia is not a specific disease and doesn’t present in isolation, but is a symptom or condition that occurs as a result of other processes going on.
When a dog has anaemia there is a drop in the number of red blood cells in the bloodstream.
When there is iron deficiency in the body, red blood cells that are produced by the bone marrow may be too small, may not develop as they should, or may become reduced because of decreased production. Red blood cells are responsible for the movement and delivery of oxygen throughout the body, essential for all basic functions.
If there is a red blood cell deficiency, the entire system can be compromised. Recognising severe iron deficiency anaemia is crucial, because the underlying cause or disease can be life-threatening. Mild cases of anaemia can be easier to reverse or manage.
SYMPTOMS
Symptoms can vary from dog to dog and really depend on the underlying cause of the anaemia.
Signs of anaemia include:
- Tiredness
- Weakness
- Difficulty exercising
- Decreased appetite
- Weight loss
- Pale gums
- Rapid breathing
- Increased susceptibility to disease
- Dark-coloured, tarry stools
- Bruising
- Blood in vomit
CAUSES
There are many types and causes of anaemia, ranging from simple blood loss or the destruction of red blood cells within the body as part of a specific disease process, to the inability of the body to produce enough red blood cells.
Causes of anaemia include:
- External blood loss due to trauma
- Blood loss in the gastrointestinal tract
- Parasitic infestation, such as fleas, ticks and hookworms
- Non-infectious diseases, such as cancer, tumours and hypothyroidism
- Infectious diseases, such as bacterial infections and tick-borne diseases
- Bone marrow disease
- Kidney disease
- Nutrition and hormonal imbalances
- Exposure to toxins
DIAGNOSIS
It is crucial to identify the underlying cause of a dog’s anaemia. Various tests, depending on your dog’s symptoms and history, will be recommended.
These tests may include:
- Test for iron in the blood
- A complete blood count to identify the extent of the anaemia and evaluate the state of the red blood cells
- Packed cell volume test
- Faecal flotation to rule out hookworms
- Faecal examination to look for parasites and blood cell abnormalities
- Urinalysis to rule out urinary tract infections and to evaluate the kidneys ability to concentrate urine
- Chemistry tests to evaluate kidney, liver and pancreatic function, as well as sugar level
- Electrolyte tests to ensure your dog isn’t dehydrated or suffering from an electrolyte imbalance
- Specialised tests that can help identify underlying infectious disease
- Bone marrow aspiration – a procedure to collect and examine bone marrow
Related Article
Anaemia Due To Iron Deficiency In Cats Read Now







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Anaemia Due to Iron Deficiency in Cats

OVERVIEW
Anaemia is not a specific disease and doesn’t present in isolation but is a symptom or condition that occurs as a result of other processes going on. When a cat has anaemia there is a drop in the number of red blood cells in the bloodstream.
When there is iron deficiency in the body, red blood cells that are produced by the bone marrow may be too small, may not develop as they should or may become reduced because of decreased production. Red blood cells are responsible for the movement and delivery of oxygen throughout the body, essential for all basic functions.
If there is a red blood cell deficiency, the entire system can be compromised. Recognising severe iron deficiency anaemia is crucial, because the underlying cause or disease can be life-threatening. Mild cases of anaemia can be easier to reverse or manage.
SYMPTOMS
Symptoms can vary from cat to cat and really depend on the underlying cause of the anaemia.
Signs of anaemia include:
- Tiredness
- Weakness
- Difficulty exercising
- Decreased appetite
- Weight loss
- Pale gums
- Rapid breathing
- Increased susceptibility to disease
- Dark-coloured, tarry stools
- Bruising
- Blood in vomit
CAUSES
There are many types and causes of anaemia, ranging from simple blood loss or the destruction of red blood cells within the body as part of a specific disease process, to the inability of the body to produce enough red blood cells.
Causes of anaemia include:
- External blood loss due to trauma
- Blood loss in the gastrointestinal tract
- Parasitic infestation, such as fleas, ticks and hookworms
- Non-infectious diseases, such as cancer, tumours and hypothyroidism
- Infectious diseases, such as bacterial infections and tick-borne diseases
- Bone marrow disease
- Kidney disease
- Nutrition and hormonal imbalances
- Exposure to toxins
DIAGNOSIS
It is crucial to identify the underlying cause of a cat’s anaemia. Various tests, depending on your cat’s symptoms and history, will be recommended.
These tests may include:
- Test for iron in the blood
- A complete blood count to identify the extent of the anaemia and evaluate the state of the red blood cells
- Packed cell volume test
- Faecal flotation to rule out hookworms
- Faecal examination to look for parasites and blood cell abnormalities
- Urinalysis to rule out urinary tract infections and to evaluate the kidneys ability to concentrate urine
- Chemistry tests to evaluate kidney, liver and pancreatic function, as well as sugar level
- Electrolyte tests to ensure your cat isn’t dehydrated or suffering from an electrolyte imbalance
- Specialised tests that can help identify underlying infectious disease
- Bone marrow aspiration – a procedure to collect and examine bone marrow
Related Article
Anaemia Due To Iron Deficiency In Dogs Read Now







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Rabies In Pets

Whenever you hear the word ‘rabies’ you should pay attention. Mammals – for our purposes humans, dogs and cats – can all get rabies.
WHAT IS RABIES
Rabies is a deadly virus and survival is highly unlikely.
Once contracted it may affect the spinal cord and cause inflammation in the brain.
However, growth starts in the muscle tissue before attacking the nervous system and spreading.
HOW IS RABIES TRANSMITTED?
Once the virus has reached the nervous system (spinal cord and brain) it heads for the saliva glands. Large amounts of the virus-containing saliva is produced and discharged into the mouth. This is why the disease is mostly transmitted through a bite.
When an infected animal’s saliva gets into an open wound, or makes contact with mucous membranes, transmission is almost inevitable. Even a scratch can cause infection.
WHICH ANIMALS ARE KNOWN TO TRANSMIT RABIES?
Wild animals pose the greatest threat to your pets in terms of exposure to rabies. In South Africa the bat-eared fox, black-backed jackal and yellow mongoose are common suspects.
COMMON SYMPTOMS OF RABIES IN INFECTED PETS
There are two forms of rabies: paralytic and furious. Mild signs will be noticeable in the first three days after infection. From here it progresses to either the furious stage, the paralytic stage, or a combination of the two. Some may even die before showing symptoms.
The virus can lead to radical physical and behavioural changes in DOGS and there are multiple phases in terms of symptoms.
Infected dogs may seem:
- Restless
- Feverish
- Anxious/Fearful
- Irritable (often the friendly dogs)
- Submissive (often in excitable dogs)
- Aggressive: snapping at/biting other animals, humans and even objects
- Obsessed with area where transmission occurred: licking, biting and chewing
- Hypersensitive to any stimuli including light, sound and touch
As the virus progresses, you will likely also notice:
- Weakness
- Fear of water
- Dilated pupils
- A tendency to hide in dark places
- Heavy breathing and jaw hanging open
- Sounds and motions associated with choking
- Loss of appetite and pica (eating of unusual things)
- Difficulty in swallowing and loss of control over the throat
- Staggering and/or paralysis of hind legs
- Disorientation or lack of coordination
- Trembling and seizures
- Foaming at the mouth
- Sudden death
The virus can lead to radical physical and behavioural changes in CATS and there are multiple phases in terms of symptoms.
Look out for any, or a combination, of the following:
- Fever
- Seizures
- Paralysis
- Weakness
- Aggression
- Dropped jaw
- Fear of water
- Extreme excitability
- Lack of coordination
- Hiding in dark places
- Pica (eating of unusual things)
- Unusual shyness or aggression
- Difficulty or inability to swallow
- Paralysis in the mandible and larynx
- Excessive, dripping saliva or frothy saliva
- Constant irritability/changes in attitude and behaviour
INCUBATION PERIOD
Once the virus has been contracted, it can take anything from one day, two to eight weeks, between one and three months, or even up to a year before symptoms appear. After that the virus doesn’t hold back.
WHICH DOGS ARE MOST AT RISK?
- Unvaccinated dogs
- Dogs that are allowed to roam on their own
- Dogs that come into contact with wild animals or pets that haven’t been vaccinated
DIAGNOSIS
There are no accurate tests except a direct fluorescent antibody test (using brain tissue) which can only be performed after death.
If you cannot safely transport your pet to the veterinary, get in touch with animal control services for assistance to avoid getting infected.
PREVENTION
- No 1: VACCINATIONS
- Supervision when outdoors
- Avoid contact with/exposure to wild animals
If you suspect that your pet has been exposed to the virus (especially if you notice any of the mentioned symptoms) take your pet to the veterinarian immediately.
Wear gloves and stay away from your pet’s mouth.
HUMAN CONTACT WITH AN INFECTED ANIMAL
If you suspect infection, seek medical care immediately as the disease is deadly and survival is rare.
TREATMENT
There is no cure for rabies. If an animal does not succumb to the disease quickly, euthanisation is considered the best course of action.
Finally, DON’T try to handle or capture a possibly infected animal (report it) and ALWAYS make sure your pets are up to date with their vaccinations.
Related Articles
What Are Pet Vaccines And Why Are They Important Read Now
World Rabies Day -Awareness & Prevention Efforts Read Now
Rabies: Diagnosis, Prevention & The Value Of Vaccination Read Now
Be a Good Puppy Owner, Don’t Miss Vaccinations Read Now
Rabies: How It Spreads, The Signs & Why Vaccination Is Vital Read Now

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
ENLARGED HEART (DILATED CARDIOMYOPATHY) IN CATS

Did you know that feline heart disease is just as dangerous in cats as it is in people?
WHAT IS AN ENLARGED HEART?
The heart has four chambers: two chambers at the top, the right and left atrium; and two chambers at the bottom, the right and left ventricles.
An enlarged heart or dilated cardiomyopathy (DCM) is a heart disease that affects the ventricular muscle. It is characterised by dilated, or enlarged heart chambers, and reduced contraction ability.
This increase causes the heart to become overloaded, the contractions of the heart weaken and therefore blood is not pumped through the body efficiently.
Typically, the heart stretches and enlarges, which over time further decreases its ability to pump blood around the body resulting in possible congestive heart failure (CHF).
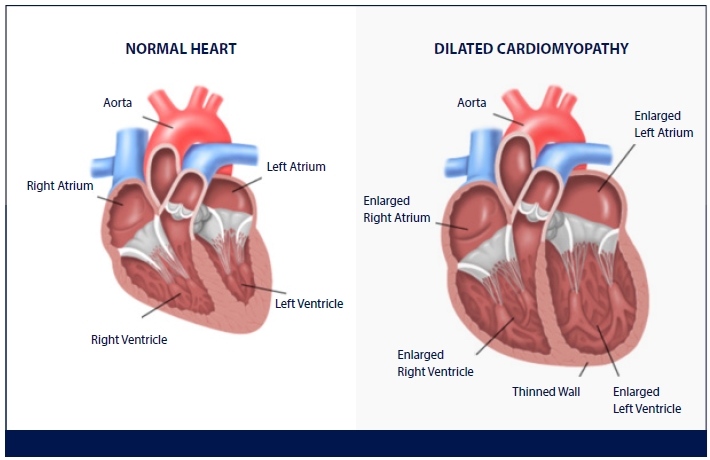
CAUSES OF FELINE DCM
The underlying cause in the majority of DCM cases today remains unknown. In some families of cats, a genetic predisposition has been identified.
More commonly affected breeds:
- Burmese
- Abyssinian
- Siamese
Ages of cats affected:
- The disease will usually affect cats between the ages of 2 to 20 years.
- The average age of onset is ten years old.
SYMPTOMS OF DCM IN CATS
Cats with enlarged hearts will often have a broad range of symptoms, and depending on the age of the cat, these could be mistaken for simply a sign of being elderly.
Only veterinary examination can pinpoint DCM for certain.
The symptoms may include:
- Listlessness (depression)
- Lack of appetite
- Weakness/sluggishness
- Exercise intolerance
- Partial paralysis as blood clots become more common
- Abnormal heart rhythm
- Difficulty breathing, possibly with a cough
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
HEART DISEASE IN CATS

We don’t want to know or think about it, but cats, just like people, can also suffer from heart disease. Any disease that affects the heart muscle is called cardiomyopathy and can lead to heart failure.
Cardiomyopathies are classified according to the effect they have on the heart muscle:
- Hypertrophic cardiomyopathy (HCM): the volume of blood in the heart is reduced and the heart muscle can’t relax properly between contractions.
- Dilated cardiomyopathy (DCM): enlargement of the heart causing ineffective contracting.
- Restrictive cardiomyopathy (RCM): the wall of the heart becomes stiff and inelastic which prevents the heart chambers from filling normally.
- Intermediate cardiomyopathy (ICM): more than one type of disease is present, for example hypertrophy and dilatation.
SIGNS OF HEART DISEASE IN CATS
There are similarities between how heart disease presents itself in cats and dogs, but there are also exceptions. Cats can often hide symptoms better which means it takes longer to detect the problem. There are signs you should look out for.
To help, consider these questions:
- Is your cat more restless than usual?
- Does your cat seem weak, less playful or does she tire easily?
- Has your cat recently fainted or collapsed?
- Is your cat’s abdomen swollen (bloated)?
- Have you noticed a decreased appetite?
- Has your cat become withdrawn or does she seem depressed?
- Is your cat struggling to walk normally, specifically with her hind legs? It could be thromboembolisms (blood clots).
- Has your cat’s breathing become laboured? Do you notice shortness of breath or rapid breathing?
- Has your cat been vomiting?
If more than one sign is significantly present, contact your veterinarian and arrange a checkup. Your kitty’s heart health depends on it!
Should your veterinarian recommend surgery, ask about treating anticipated pain to help your cat feel more comfortable after the procedure.
Related Articles

HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Facts About Your Cat’s Eyes

Cats are weird, wonderful and rumoured to be wise… especially when you look in their eyes! But, how do they actually view the world around them? Well, science has come up with a few generally agreed upon facts to help us understand this interesting feline organ.
But, before we jump into feline eye facts, let’s take a look at eye anatomy first:
- Light enters the eye through a lens.
- Behind the lens of each eye there is a pupil (essentially a gateway to the retina).
- The retina sits at the back of the eye.
- Via the optic nerve, the retina transports images and light to the brain.
- The brain turns all this information into a visual we can understand.
- The retina has two types of receptors: ones that detect light (called rods)
and ones that detect colour (called cones).
LOW LIGHT YES, PITCH-BLACK DARK NO
Somewhere along the line, many of us have heard that cats can see in total darkness. Unfortunately for them, this is not true. They do however only need one-sixth of the light we need to function. How is this possible?
Reason number one: they have more rods (receptors that detect light).
Reason number two: a certain tissue located at the back of the eyes allows light to reflect within the eye, enhancing sight. This same tissue is responsible for the slightly sinister shine that’s visible when we spot a cat in the dark
LIMITED ‘RAINBOW’ VISION
Distinguishing a variety of colours is not one of their strengths, however, they’re not totally colour blind. Compared to humans, they have fewer cones (receptors that detect colour) and these cones are less concentrated as well. Apart from not experiencing the intensity of hues, scientists reckon that greens and reds can’t be distinguished, while yellows and blues are clearer.
THE DEVIL IS NOT IN THE DETAIL
Although cats are not able to visualise the same amount of detail humans do, they’re not nearsighted (that is, they don’t have a vision problem related to lens shape defects). Instead, the amount of detail is affected by how the rods and cones work together. Compared to humans, objects such as leaves and text on a page are perceived differently. The fact that a cat’s lens shape remains unchanged in terms of close-up focus have many researchers convinced that cats are farsighted, with optimal vision up to 90 cm.
THE VALUE OF VERTICAL PUPILS
Pupils shaped like vertical slits are found in animals that are both diurnal and nocturnal.
The reason: This shape is able to facilitate faster pupil change. The reduced pupil size is also less affected by sudden light level changes as less light enters the lens.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
KIDNEY TOXICITY IN DOGS
WHAT IS KIDNEY TOXICITY (DRUG-INDUCED NEPHROTOXICITY)?
Like human kidneys, a dog’s kidneys balance certain substances in the blood and filter out and excrete the body’s wastes as urine.
Some drugs administered for the purpose of diagnosing or treating another medical disorder may have toxic effects on a dog’s kidneys.
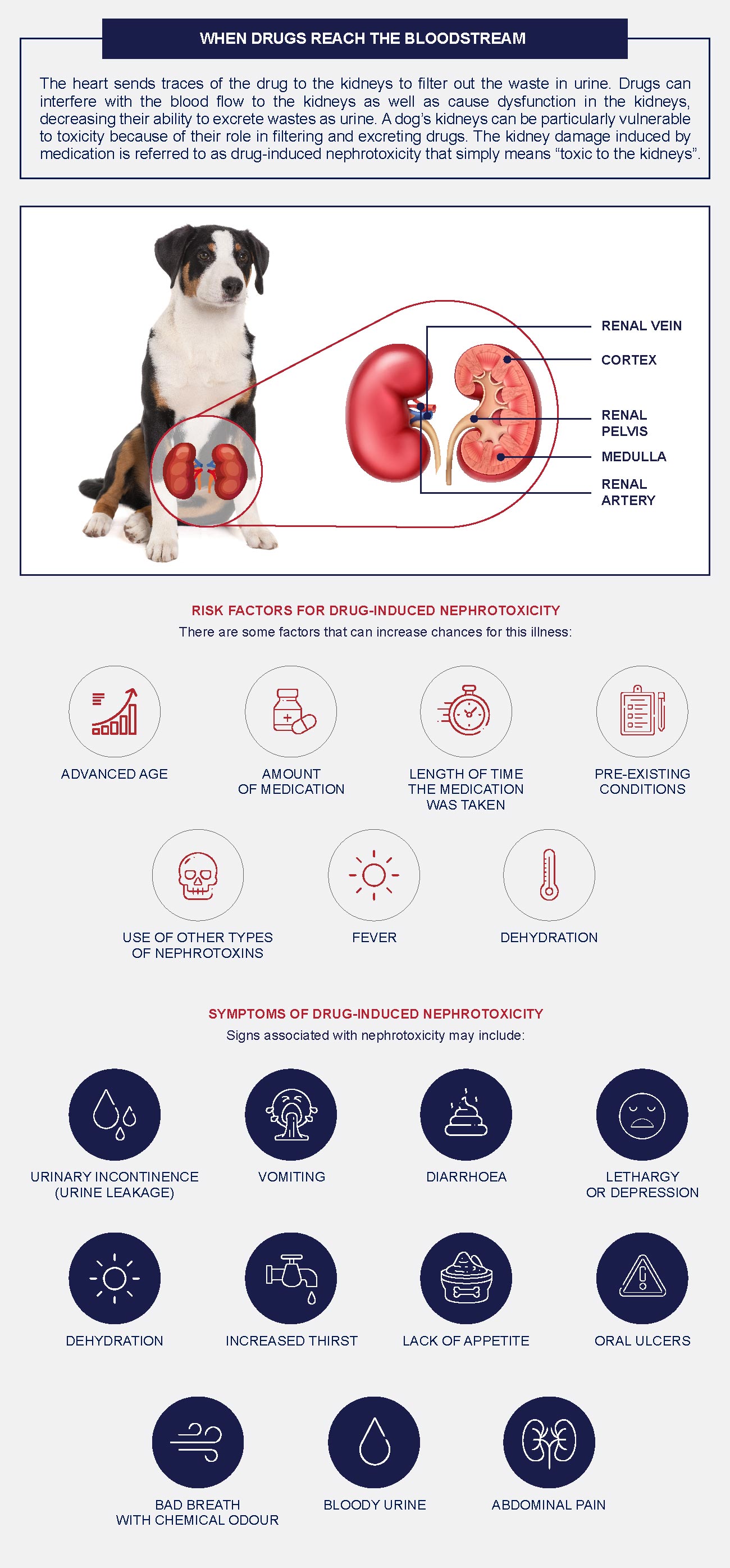
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
ANXIETY IN DOGS – FEARS & PHOBIAS

Anxiety or fear is the feeling that something bad or unpleasant will happen. It is related to uneasiness, nervousness, restlessness, tension and dread.
When it feels like a situation, person or object is posing a threat, whether real or believed, an instinctual anxiety can be experienced which causes the body to prepare for freeze, fight or flight (flee) mode. This behaviour is usually seen as normal and necessary for adaptation and survival, unless the fear response is abnormal or inappropriate (it depends on the context). It’s believed that most abnormal reactions are not natural, but instead learned, which means it can be unlearned.
If the fear of something or someone is constant and almost uncontrolled, it is called a phobia. Often the memory of, or incidences associated with a phobic event, can cause a response in a dog.
Noise related occurrences, for example thunderstorm and fireworks, are linked to common phobias.
On the other hand, anxiety refers to the anticipation of future threats which can either be unknown or imagined. The associated fear can cause normal and visible body-related reactions such as urination and/or passing of bowel movements, destruction, barking or crying.
The most common anxiety that dogs can suffer from, specifically when they are alone, is separation anxiety which reveals itself in stress behaviours.
Between one to three years of age, when a dog is socially mature, the majority of anxieties, fears and phobias develop. The cause is unknown, but significant fear and withdrawal can also occur between eight to ten months of age. Older dogs may also eventually suffer from separation anxiety and though the cause is not clear, it could simply be related to age and natural regression.
ANXIETY SYMPTOMS & TYPES
- Fight or flight behaviour (driven by the sympathetic autonomic nervous system) and signs which may include diarrhea.
- Mild fears can cause trembling, withdrawal, hiding, tail tucking, a decrease in activity, as well as passive escape behaviours.
- Panic can cause active escape behaviour or an increase in movement, which may seem strange and can be harmful to the dog.
- Anxieties: lesions caused by licking and/or biting of self (secondary to anxious behaviour).
WHAT CAUSES FEAR AND ANXIETY IN DOGS TO DEVELOP OR INCREASE?
- Illness or pain.
- Terrible, frightening and/or unfamiliar experience(s).
- Lack of social exposure in the first three and a half weeks of a dog’s life.
- Memories related to the inability to escape a space or stimulus (e.g. being locked up).
- Toxic conditions (e.g. lead poisoning); infectious disease, usually viral (which can compromise the central nervous system); and nervous system changes associated with ageing.
- Having experienced separation, whether it’s related to abandonment, having multiple owners, re-homing or neglect (or even worse: abandonment or re-homing because of the dog’s separation anxiety).
DIAGNOSING DOGS
A dog’s behaviour can be influenced by disease (e.g. brain or thyroid), or toxins, so your veterinarian will first do tests. If fear, anxiety or phobia is suspected, behavioural techniques can be recommended or prescribed medication. The choice will depend on the individual dog, its fear trigger and the owner.
CALMING AN ANXIOUS DOG
In extreme cases, if medication is not available or effective yet, hospitalisation could help. It might not be cost-effective, but not everyone has time to care for their dog at home, often protecting them from self-inflicted injuries and other worrisome behavioural problems.
Another alternative is hiring a qualified pet sitter with the relevant experience since a doggy day care could just aggravate the situation.
A combination of medication and behaviour modification could work. If you notice itching and/or pain, you have to intervene and try to control the discomfort. Also, keep your dog away from social stressors and only allow access to a non-threatening, protected environment that’s not too large or confined.
Modifying behaviour is difficult, but possible. When your dog seems panicked, don’t offer reassurance because it may be understood as a reward for his or her behaviour. Instead, encourage calmness. Need to know: for some dogs, a crate is a safe place; for others it’s a prison. Most importantly: don’t punish behaviour caused by fear, phobia, or anxiety.
Essentially you want to reduce the action caused by the trigger (e.g. isolation in a dark space) and early treatment can make a big difference.
You can either use desensitisation: expose your dog to the fear-inducing stimulus repeatedly, but in a very controlled manner so that eventually an undesirable response is avoided.
Alternatively, try counter-conditioning: train your dog to react positively instead of showing fear or anxiety when confronted with the fear-inducing stimulus.
Example: try a sit-and-stay reward system and use this when your dog is showing signs of acting out. In this way, you can take control of rising anxiety and turn the situation into something positive.
HOW TO LIVE WITH AND MANAGE ANXIETY IN DOGS
Dogs on anxiety medication should be monitored and taken to the veterinarian for a follow-up visit.
If behaviour modification doesn’t seem to work, medication should probably be considered because the disorder can progress. Just remember that any treatment can take time to be effective, meaning anything from a minimum of six months or possibly years. The duration, intensity and amount of symptoms will play a role.
HOW TO PREVENT ANXIETY AND FEAR IN DOGS
Puppies should be exposed to social situations that include other people and other dogs (possibly other pets, if you think it’s safe).
This should be done before 14 weeks of age for the best results.
If puppies do not socialise it’s likely that fearful behaviour will develop. Just a little bit of exposure can really help to avoid this possibly long-term problem.
Related Articles







HEALTH & WELLNESS

TRENDING

We’re excited and honoured to feature South Africa’s second largest independent animal welfare organisation on PetlifeSA.
Rabies: How it spreads, the signs & why vaccination is vital

Rabies is a zoonotic viral disease, meaning a disease that normally exists in domestic and wild animals that can infect humans. It attacks the central nervous system and once symptoms develop, it’s almost always fatal.
HOW RABIES SPREADS
Both domestic and wild rabid animals can transmit rabies to healthy animals and humans when their saliva comes into contact with broken skin or mucous membranes.
Contact usually occurs through a bite, scratch or lick. In Africa and Asia, jackals and mongooses are the main wildlife reservoirs for the rabies virus.
There are two types of rabies and a combination of symptoms may be experienced:
- Furious Rabies: Hyperactive Symptoms
- Paralytic Rabies: Weakness and Loss of Coordination
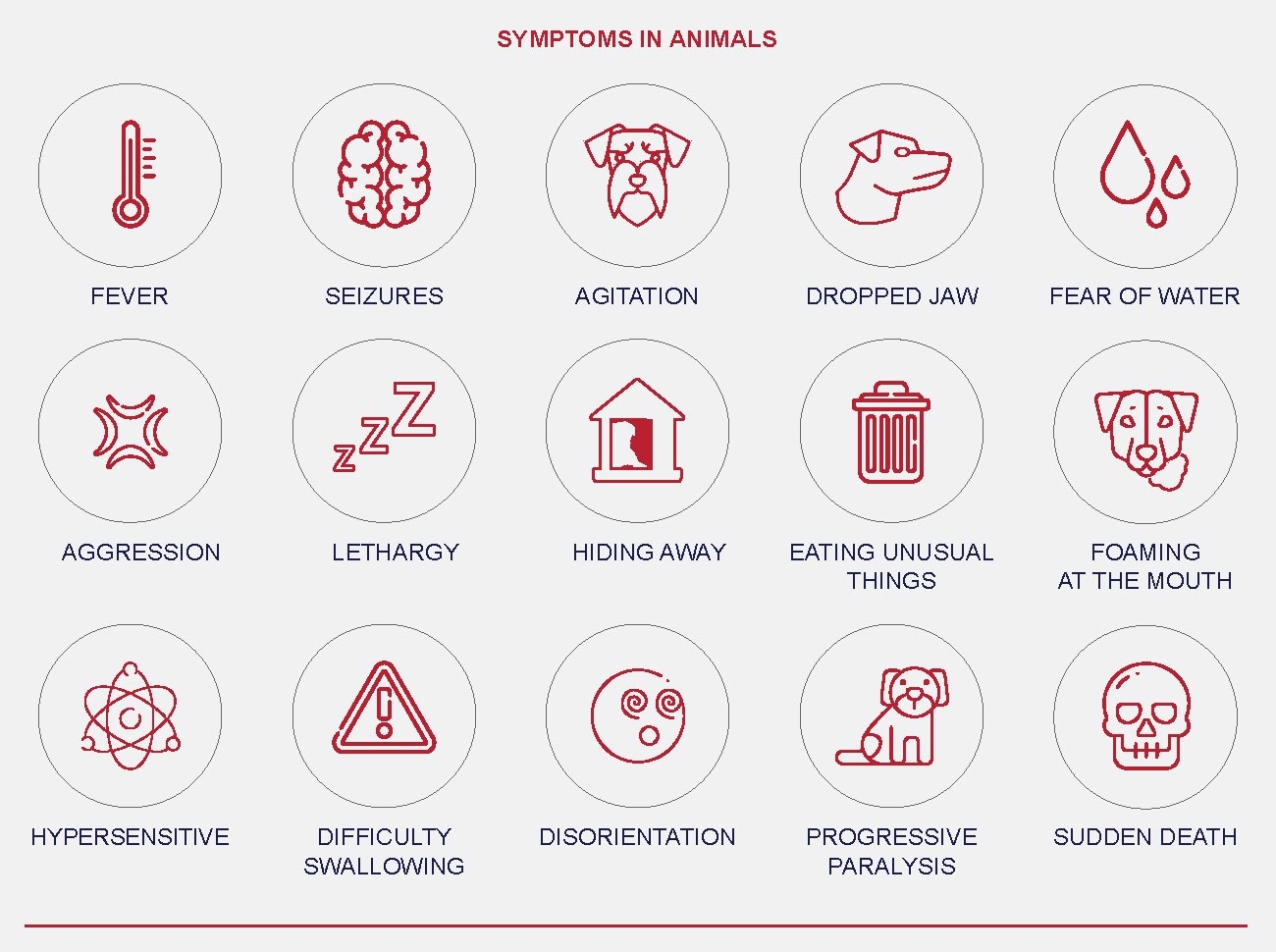

WHAT TO DO IF YOU HAVE BEEN BITTEN BY A DOG
- Wash the wound with running water thoroughly for 10 minutes.
- If the dog is unvaccinated, go to your doctor or clinic immediately to start rabies vaccinations.
- Do not wait for symptoms to appear before going to the doctor. Once symptoms appear, it is too late for treatment.
WHY VACCINATION IS VITAL
Vaccination is vital because this deadly disease is 100% preventable.
- Rabies is deadly
- Rabies is 100% preventable
- 40% of rabies victims are children younger than 15
- Every year, tens of thousands of people die from rabies
- Rabies is an endemic in more than 150 countries and territories
- Africa and Asia account for 95% of human rabies deaths, worldwide
- Dogs are the main source of human rabies death: up to 99% transmission rate
DOG VACCINATION IS THE MOST EFFICIENT WAY TO ELIMINATE HUMAN RABIES
By preventing rabies in pets, you help them live longer, happier lives AND you help keep loved ones and others in your community safe.
Do not buy or adopt pets if you cannot afford vaccination.
Related Articles